One side of the sign on Dr. Osman Ipsiroglu’s office door welcomes visitors; the flip side says, “I’m not in, or I’m power napping.” Just plain napping at the office is not acceptable in our culture, he says, but power napping, a concept that came from Wall Street, is. It’s a wry acknowledgement, from someone who should know, that sleep today is complicated.
Ipsiroglu runs a sleep clinic at Sunny Hill Health Centre, a rehabilitation facility for children with disabilities, on a quiet street in East Vancouver. He brews tea in a graceful old pewter pot and tells me about the troubled relationship between children and sleep. “We focus on waking behaviours,” he says of his profession, “and we don’t have a concept of how to treat real sleep problems.”
As we sip our tea, there’s a knock on the door. Elizabeth, one of Ipsiroglu’s patients, enters with her mother, Claire. Elizabeth is a charismatic eight-year-old, dressed in purple—glasses, sweater, and a scarf lit with glints of silver. The doctor compliments her on her colour coordination and leaves Claire to tell their story. (Some names have been changed and surnames omitted to protect the anonymity of sources.)
Following a difficult pregnancy—the baby seemed never to stop moving and was born early—Claire was unable to soothe her first-born: “She was driven by a motor.” She couldn’t settle, stopped napping before she was a year old, never slept for more than a few hours at a time, and needed her parents to lie on top of her to keep her still (“Which I like!” Elizabeth adds).
Out of desperation, the parents were sleeping in bed with their child. By the time Elizabeth was nine months old, Claire and her husband, Dan, were exhausted emotionally and physically, and found themselves unable to stick to the standard sleep techniques. Their daughter was getting eight hours a day at most; a child of her age typically gets fourteen.
When Elizabeth was three, social and emotional lags became apparent. “Alarm bells were starting to go off,” says Claire. She and Elizabeth began seeing an infant psychiatrist in Burnaby. The problem was a lack of sleep, but she had developed other behavioural issues that were more worrying. Elizabeth had several different diagnoses, including anxiety, a developmental coordination disorder, and attention deficit hyperactivity disorder. (Children with chronic sleep deprivation are often misdiagnosed with ADHD, as both conditions result in distracted, frenetic, and grumpy kids.) The ADHD medication exacerbated Elizabeth’s difficulties, making it even harder to fall asleep. In addition, she developed a facial tic, and her emotions ricocheted up and down. When she told her mother, “My brain is crying,” the family discontinued the medication.
By the time Elizabeth entered kindergarten, she exhibited significant motor challenges. Using scissors, negotiating monkey bars, and holding a pencil were all beyond her. Claire—demoralized by psychiatrists who seemed to think the problems stemmed from her presumed failure to attach to her daughter, bruised from nighttime thrashing, and seriously worried about the future—says she was in her “lowest space ever as a mom.”
Ipsiroglu, who trained in Austria, is a rarity among doctors, in that he specializes in sleep. Only 25 percent of American doctors spent more than six hours on the subject during medical school. In the United Kingdom, the median time spent on sleep disorders for doctors in training was five minutes. Although the field is under-recognized and underfunded in pediatrics, Ipsiroglu has one luxury at Sunny Hill: a schedule that allows him to do a two-hour history with every new patient. In order to see the problem holistically, he includes the whole family in the session.
British Columbia has only one pediatric sleep lab, in Vancouver. It’s at BC Children’s Hospital, and it’s capable of conducting polysomnograms—sophisticated all-night studies, carried out in the hospital, which track and measure movement, oxygen saturation, brain waves, carbon dioxide levels, and more. Failing that, Ipsiroglu uses a home-based system that he couriers around the province. He records his patients “where sleep happens, at home,” on an inexpensive video machine. “I don’t see the brain waves, but I see whether the child is awake or asleep, when he falls asleep, whether he is restless, how he wakes up, how long it takes him to fall asleep again.” He also sees night terrors and the frequent parent-child interactions that punctuate fitful nights.
Elizabeth was five when the family was sent to Ipsiroglu. “We came to him with nearly three years of psychiatric documentation,” Claire recalls. “This kid had been looked at from every angle, and yet the picture was still not coming together.” The doctor’s interest in the family’s history struck Claire as both novel and heartening. He had a strong hunch from the history alone that this was a “textbook story” of the neurological syndrome called Willis-Ekbom, or restless leg, and the home videotapes confirmed it. (Elizabeth recalls of the video, “And I scratched my bum!”) Ipsiroglu thought that Dan, a lifelong poor sleeper, might also have a serious case of restless leg, and that Claire may be on the spectrum.
Suddenly everything made sense. Restless leg syndrome, which is highly hereditary and affects 1 to 10 percent of the population, is difficult to diagnose in children because they can’t articulate their constant sense of physical irritation, if not outright pain. Now Elizabeth’s inability to rest, her need for deep pressure, her compensatory sucking, and most other coping mechanisms were explained. She started taking a neuropathic pain medication and getting lots of exercise; before long, she snuggled up to her mother for the first time in her life and said, “My body is not screaming to my brain.”
Between private assessments, attachment-focused play therapy, and the educational assistant who accompanied Elizabeth to kindergarten, the family has spent more than $100,000, a figure that includes the income lost when Claire had to give up work to care for her daughter. Relaxation, sleep, and improved coordination swiftly followed the restless-leg diagnosis. What have taken longer to correct are the girl’s anxiety and challenges with reading social cues and nuances.
“We’ll never know whether her anxieties or learning difficulties were there from the start, or whether she learned the anxieties and problems from the sleep deprivation,” Claire says. “My intuition as a mom is that she did.” Recalling how as a preschooler Elizabeth was trucked around from appointment to appointment, her mother says, “That shapes how you see yourself in the world, and I think there will be an enduring sense of, I’m not doing things right.” Ipsiroglu’s emphasis on the whole family helped alleviate that feeling: when Elizabeth learned that her father also had restless leg, she felt as if a weight had been lifted from her shoulders. She said, “Well, it’s okay, because you have it too, and we’re going to deal with it.” She felt like part of the family again, no longer an outlier who was causing trouble.
Hiding more or less in plain sight, Elizabeth’s diagnosis took three years to make. Her physiological obstacles are now being managed, but she still belongs to what William Dement, one of the fathers of sleep medicine, calls “a sleep-sick society.” School-aged kids are going to bed later and later, averaging seventy-five fewer minutes of sleep per night than they did at the start of the twentieth century. Teenagers in particular are perilously deprived: studies estimate that as many as 40 percent aren’t getting enough sleep. Surveys and public-health organizations tell us that sleep deprivation in children is now an epidemic. Yet underslept kids, who are susceptible to developmental delays and assorted health issues, often are misdiagnosed, just as Elizabeth was.
Even losing a little sleep can have measurable consequences. One study found that a group of young children showed lower levels of cortisol—a hormone that helps with stress and pain management—after they’d missed their nap. Because more growth hormones are released during slumber than at any other time, the physical development of a tired child also may be affected. Studies have connected inadequate sleep to weight gain, cardiovascular problems, diabetes, compromised immunity, and emotional and social issues. Moreover, research has shown that deprivation early in life can affect later cognitive performance and neuro-developmental functioning—something particularly worrying in the case of Elizabeth, who may well have trouble concentrating, behaving, controlling her moods, and avoiding accidents and injuries.
The reasons kids aren’t getting enough rest are various—they range from neurological problems to the siren calls of smart phones and tablets—but almost all the obstacles to sleep would be treatable if we were willing. Underlying those challenges is something more fundamental, as the sign on Ipsiroglu’s door suggests: a profound lack of respect for sleep. Our culture glorifies people who get very little. Former French president Nicolas Sarkozy boasted that he worked so hard he barely slept. Margaret Thatcher’s “sleep is for wimps” still resonates, as does Donald Trump’s question, “How does somebody that sleeps twelve and fourteen hours a day compete with somebody that’s sleeping three or four? ” Not all the boastfully underslept examples are workaholics, and at least one, Michelle Obama, is notably health conscious. When she rises at 4:30 a.m., she sends the message that rest is the first and perhaps the only thing we can eliminate from our busy lives. In our non-stop world, sleep is out of step. Sleep is for losers. Sleep is just too, well, dozy.
Five-year-old Blair is wearing Superman socks and hockey pyjamas and has long, thick eyelashes. A Little Mermaid doll reclines on the bed next to him. The boy’s brother Noah, eight, is watching Rescue Bots on an iPad; his brother Jacob, one, is busy opening and closing drawers; his parents are doling out slices of banana bread.
Blair wants his father’s tablet.
“Only because you’re here,” his father, Will, tells him, as he hands it over.
“Here” is a room in Toronto’s Hospital for Sick Children, where Blair is being prepared for his second polysomnogram. His mother, Robin, is filling out a hospital questionnaire.
“Blair, are you still tired in the morning? ”
“Yes,” he says, not looking up from the tablet, on which he is watching Frosty the Snowman. Meanwhile, Debra Medin, his respiratory therapist, is taping wires to his big toe (to monitor his oxygen levels), and to his calves and pyjama legs (to record movement). Two belts, strapped around his chest and abdomen, will monitor his breathing. Holding the tablet up in the air with both hands, he pays little attention to the accumulating strands and straps.
A prodigious snorer, Blair often was sick as a baby. At three years old, he had pneumonia in both lungs and was prescribed puffers. They didn’t work. Last year, he missed more than fifty days of school. Small and pale, he would drift off in the car, sometimes twice a day. He also began to exhibit symptoms of obsessive-compulsive disorder, closing the garbage can and then tapping it twice, making sure that the kitchen stool stood in a particular place. None of it added up, and no pediatrician or ear, nose, and throat specialist asked about snoring, which Robin now knows is a red flag that signals the possibility of obstructive sleep apnea.
Finally, eighteen months after his double pneumonia, he was sent to a respirologist. Filling out the questionnaire, Robin recalls, “I just went, yup, yup, yup. It was the first time it all seemed to fit.” The respirologist sent Blair to a new ear, nose, and throat specialist, who suspected the boy had sleep apnea and needed to have his tonsils and adenoids removed. But his mother decided she was not going to subject her son to general anaesthetic and surgery without first being sure that the doctor was correct, and only a polysomnogram could provide that certainty.
That’s when she came face to face with the increasingly overstretched resources of the lab at SickKids. Or, to put it another way, that’s when the lab came face to face with Robin’s tenacity. Told she might have to wait up to eighteen months for a study, she began calling every few days, hoping for a cancellation. After two and a half weeks, a call came: Could they come in three hours? They could.
The results of a polysomnogram typically arrive in six to eight weeks. Blair’s came in twenty-four hours. A person is considered to have severe obstructive sleep apnea when there are ten or more apneas, or temporary breathing stoppages, per hour. Blair’s first study counted forty-nine. “That was alarming,” his mother says, not only because the disorder brings with it the risk of cardiovascular and blood-pressure problems, but also because it was distressing to realize how much her son struggled to breathe while he slept.
A month later, in May 2014, Blair had his massive tonsils and even more massive adenoids removed. In the six months after his surgery, he gained almost ten pounds. Before, his sweaty, laboured sleep burned a lot of calories. Afterwards, he still snored, but much less, and less loudly. Even some of his obsessive-compulsive behaviours—which have been known to accompany sleep apnea—disappeared. The stool he once needed to keep in its special place could stand anywhere in the kitchen. This second study, which I am now observing, will evaluate the extent of his recovery.
After forty minutes’ work by Medin, nearly everything about Blair’s sleep that can be measured is ready to be measured. Outfitted with nose prongs, and with his head wires secured in a stocking cap, he looks like a high-tech Smurf. He says good night to his mother and brothers; his father will stay with him. Down the hall, in a monitoring room, screens show the boy settling down and closing his eyes. On another screen, a busy pattern of zigs, zags, and colour-coded geometric shapes indicates where he is in what experts call the architecture of sleep. A technologist decodes the pattern: “Now he’s in stage one, the relatively light phase, and now he’s in stage two,” the transitional state between light and heavy slumber.
The polysomnogram shows that Blair’s surgery was extremely effective, having improved his condition from severe to mild and reduced his carbon-dioxide levels to within a normal range. He was put on medication for three months to reduce any residual swelling, and possibly even to eliminate the problem completely. His brother Noah also has undergone surgery for sleep apnea, and Robin suspects that Jacob has the disorder too. She has just one wish: that doctors would ask at regular checkups, “Does your child snore? ”
“If that had happened,” she says, “likely my children would have been helped years earlier.”

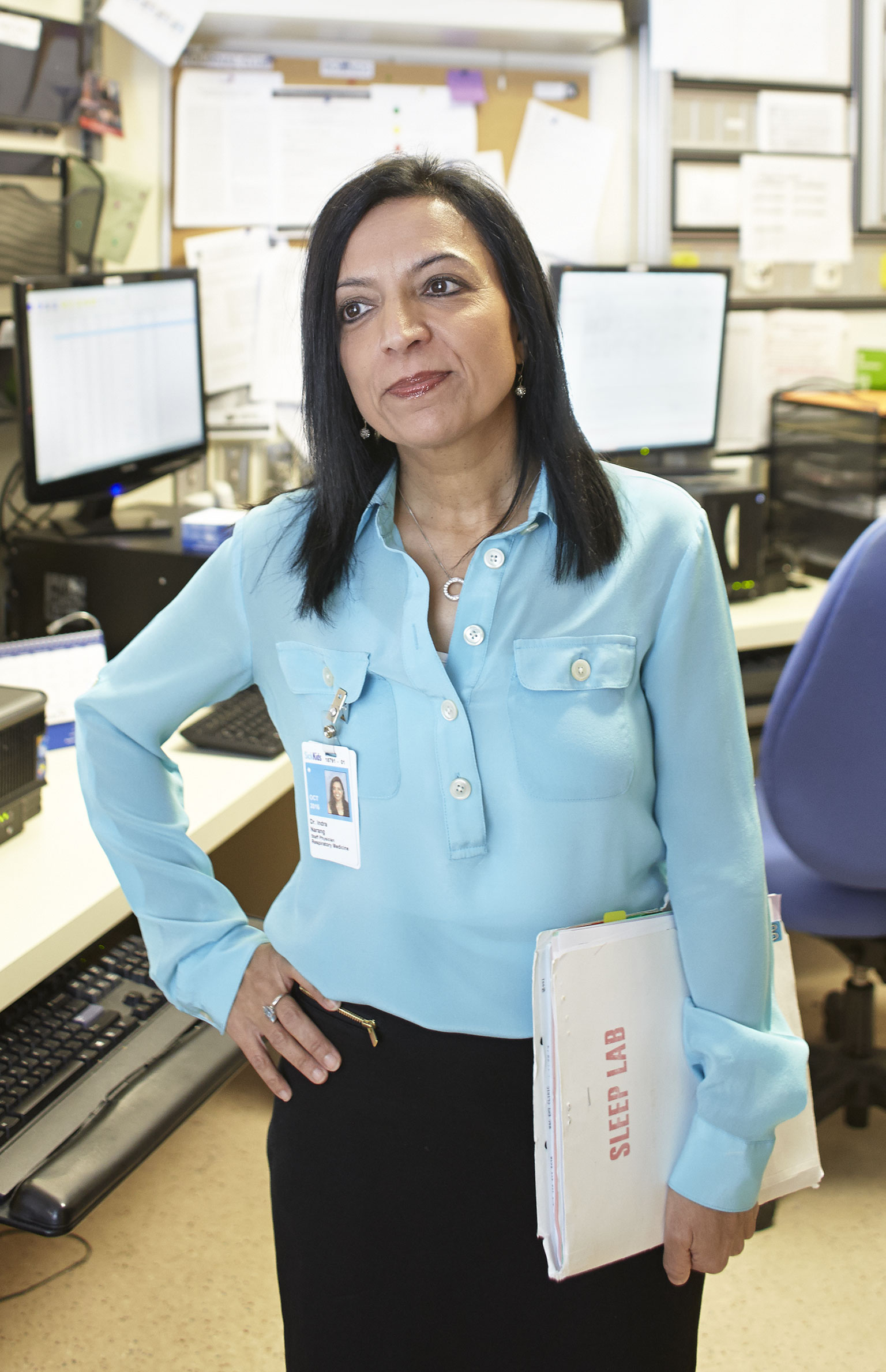
The SickKids lab handles everything from severe, life-threatening disorders to situations in which a child and his or her family need nothing more complicated than coaching in proper sleep hygiene. “We’ll take anything,” says Dr. Indra Narang, the director of sleep medicine. But taking anything is becoming increasingly difficult.
Compared with pediatric sleep medicine in the United States, she says, Canada is “the poor neighbour.” Our country isn’t training or importing enough sleep specialists. The SickKids lab has expanded since Blair’s mother was told to expect an eighteen-month wait, but the average wait is still six months. (In a major American city, the wait would be three months.) In Vancouver and Calgary it’s twelve months; in Ottawa, up to two years. Halifax no longer has the funding to conduct pediatric polysomnograms.
Meanwhile, the demand for specialists and study slots keeps rising. Until about eight years ago, Narang saw apnea, which occurs in 1 to 4 percent of healthy children, mostly in kids between two and eight years old. They would undergo studies and have their tonsils and adenoids removed, and in most cases that would be the end of their ordeal. But now, she says, “the obesity epidemic is killing us.”
Statistics Canada reckons that almost a third of children are overweight or obese, and up to 30 percent of obese children, who are usually eight or older, have sleep apnea caused by fat around the neck and stomach. (Joe, the “wonderfully fat boy” who snores and constantly nods off in Charles Dickens’s The Pickwick Papers, has a precisely observed case of obesity hypoventilation syndrome, as it is now called. In tribute to Dickens, the condition was originally dubbed Pickwickian syndrome.) Removing their tonsils and adenoids does not solve the problem, so the children need to be hooked up to a continuous positive airway pressure system—or CPAP—that keeps the airways open. Obesity combined with apnea and inadequate sleep creates a vicious cycle in which the sufferer eats more and more as fatigue stimulates his or her appetite. CPAP makes sleep easier so that the cycle can be broken.
The strain on Narang’s clinic and lab is formidable. About 1,200 patients pass through its doors every year. Even so, she believes that as many as 70 percent of obesity-related cases of sleep apnea go undiagnosed, owing to the general lack of interest in and knowledge of such disorders among medical professionals.
Most children, including Narang’s own five-year-old daughter, have no physiological barriers to good sleep, but many parents need guidance when it comes to creating a slumber-friendly environment. Narang practises at home what she preaches at SickKids. Sleep happens according to a strict schedule that doesn’t change on weekends: thirty to sixty minutes before bedtime, all technology is turned off, and it’s time for reading and quiet music. The bedroom is dark, except for a night light, and no TV is allowed in the room. All eminently sensible ideas—and easier to put into practice with a five-year-old than with a preteen or adolescent.
“I think George is tired a lot of the time,” Rosemary says of her thirteen-year-old son. “I have to wake him up every morning—he doesn’t naturally wake up—so that says to me he needs more sleep.” George is a gifted hockey player who lives with his family in Toronto. He has three practices and two games a week, plus an extra early-morning skill session at least once a week. Normally, he goes to bed between 10 and 10:30 p.m. and gets up around 7:45 a.m., except when the extra session has him up before 6. The games end at 9 or 9:30 p.m., and it’s hard for him to come down from such intense physical and emotional activity. Recalling how preoccupied she had been with the subject when her children were babies and toddlers, Rosemary says, “Sleep is one of the last things we think about—which is funny, because it used to be so important.”
George started playing hockey as a pastime, but each year it becomes more demanding and time consuming. “It’s like a train you can’t get off,” his mother says, adding that she feels an increasing sense of responsibility for her child’s athletic development. Like most of the parents on George’s team, Rosemary and her husband book their kid in for supplementary early-morning sessions. “We do it because we want them to succeed in their skills,” Rosemary says. “But it trashes their sleep.”
George has a sister, Charlotte, who is eight. She has three hours of dance class a week, plus Brownies and a piano lesson. That’s doable for a grade-three child, but because the household tends to organize itself around George’s hockey schedule (and because Charlotte likes to be close to the action), the siblings keep almost identical hours. She, too, must be woken up, and she’s often yawning and sleepy.
There’s yet another complication for these sleep-challenged kids: Their father, Paul, is an emergency-room doctor who works shifts; he’s often sleeping during the day and awake at night. When he’s home in the evening, he lets the kids stay up later so that he can spend time with them. As in most middle-class families, everybody has at least one screen: an iPhone for George, an iPod for Charlotte, iPhones and iPads for the parents, and a television. They all use these screens in the evenings.
Rosemary guesses that her son is average among his peers in terms of the amount of sleep he gets. The statistics bear her out. The US Centers for Disease Control and Prevention recommend at least ten hours for school-age children, but fewer and fewer are hitting that target. George and Charlotte are nice, sociable kids who do well in school. It helps that right now their homework is not onerous—but that will change. The thirteen-year-old daughter of one family friend has dance class almost every day after school and starts her homework well into the evening. Her mother often goes to bed before she does, and the girl regularly dozes in the car.
None of this surprises Carl Honoré, a Canadian writer who now lives in London. Honoré is the non-fiction laureate of the Slow Movement, having written In Praise of Slow: How a Worldwide Movement Is Challenging the Culture of Speed in 2004 and, in 2013, The Slow Fix: Solve Problems, Work Smarter and Live Better in a World Addicted to Speed. He also wrote a book, published in 2008, about hyper-parenting, called Under Pressure. In it, he tells the story of a California mother who bought a Palm Pilot for her son so that he could keep track of his appointments for Spanish, tennis, basketball, karate, piano, baseball, swimming, and soccer. The son was ten years old. Honoré observes that many working parents now outsource their children to after-school activities and then keep them up late so they can spend time with them.
For him, tired children are the predictable casualty of our “fast-forward, hurry-to-the-finish-line, roadrunner” culture. “Something unique is going on in this generation,” he says. “The new non-stop economy and the new technology are intersecting to make this perfect storm where something as basic as sleep becomes hard.”
Recently, for Australian television, Honoré spent a month trying to get three typically fast-moving families to slow down. More and better rest for the parents and children alike turned out to be one of the positive outcomes of the experiment. Banning screens from the home, although it elicited anguished shrieks at first, made a big difference. The writer installed a “gadget box,” and all family members were to place their devices in it upon entering their house. He introduced slower, more relaxing activities such as puzzles, board games, and at least thirty minutes of reading a day. The families spent more time eating dinner together and chatting in the evenings. Even the eight-year-old, who was addicted to his Xbox, turned into a keen reader.
Despite our stubbornly sleep-averse culture, there are people who have given us new ways to think about rest. By and large, psychologists have shown as little interest in the subject as physicians, but Reut Gruber has been preoccupied with children’s sleep, as both an investigator and an advocate, for nearly twenty years, since she was a graduate student at Tel Aviv University. For a researcher, it’s a rich field. In one study, Gruber, now a clinical child psychologist at McGill University, found that giving kids aged seven to eleven just twenty-seven minutes more sleep for five nights resulted in greater alertness and decreased impulsivity. Depriving children of an hour or so of sleep produced the opposite effect. In other studies, she demonstrated that children with greater sleep efficiency (that is, children with a higher ratio of time spent asleep to time spent in bed) do better in math and languages than children who are less efficient. She also showed that shortened and poor-quality rest are associated with increased appetite, which in turn increases the risk of obesity. When Gruber deprived children with borderline ADHD of about an hour of sleep per night for six nights and then re-examined them for the disorder, their responses resembled those typical of patients with full-fledged ADHD. That’s not to say sleep could cure the disorder, but it demonstrates—as Elizabeth and her family learned—how easily kids can be mislabelled, and how significant getting the right or wrong amount of sleep can be.
Convinced that appreciation for the importance of sleep must start at a young age, Gruber teamed up with Gail Somerville, the director of complementary services for the Riverside School Board, in Montreal, and together they led the creation of a curriculum for grades one through six. Called Sleep for Success, it’s a flexible unit that can be taught in science, mathematics, or English classes. The youngest children meet Sleepy Steven, a mischievous boy whose adventures and misadventures revolve around snoozing. Kids in grades three and four concentrate on a troupe of comic book–style superheroes called the Sleep Squad, who can use their superpowers only when they’re well rested. The oldest students follow a team of sleuths known as the Critical Sleep Investigators—or CSIs—who use the scientific method to demonstrate the advantages of getting enough shut-eye. About 900 children have participated in the optional program so far, and it has received high ratings from parents and students alike. What’s unusual about the curriculum is that it was designed not only to impart knowledge, but also to alter behaviour. And according to Gruber’s analysis, it has been a thorough success. Quantitative and qualitative measures demonstrated that children who had studied the unit fell asleep faster, stayed asleep longer, and showed improved daytime alertness and functioning. Bedtime resistance and nighttime fears were also diminished.
Teenagers are the most sleep deprived of all children. Although their late bedtimes and late risings can look like ornery egotism, in reality they are the result of adolescent brain chemistry. For reasons that aren’t yet understood, melatonin, the hormone that makes us drowsy, is released in the teenage brain about ninety minutes later than in the brains of children and adults, and it remains there longer, too. That means when a teenager has to get up by, say, 7 a.m. to get to school on time, he or she is effectively getting up in the middle of the night, which often leads to absenteeism, tardiness, and inattention. More seriously, studies have shown that teen drivers who start their day early are significantly more likely to have a car accident on the way to school. In 2014, the American Academy of Pediatrics declared that insufficient sleep constituted “the most common, important and potentially remediable public-health risk” for teens, and recommended that classes at middle and secondary schools not start before 8:30 a.m.
That target wasn’t good enough for Toronto’s Eastern Commerce Collegiate, which since 2009 has boasted the latest start time of any public school in Toronto (and probably Canada): 10 a.m. The change was championed by Cathy Dandy, who at the time was a school trustee, a mother “on my third teenager,” and someone familiar with adolescent-brain research. Eastern Commerce had a sympathetic principal, Sam Miceli, and a population that commuted from all over the city to get to school. The agreement to start classes at 10 a.m. took eighteen months of negotiations between the superintendent, teachers, and parents. The most common objection from parents and the public—in yet another example of our collective disregard for sleep—was that the school was catering to slackers and sleepyheads.
Students at Eastern Commerce are two and a half times likelier than those on a regular school schedule to get their recommended nine hours of sleep a night. Attendance is up, tardiness is down, and there have been modest gains in grades and accumulated credits. As a teacher, Heather Gillett notices the difference in the afternoons. “After lunch, the kids in other schools would be passing out; it would be really hard to teach an afternoon class,” she says. “I don’t see that dip in the afternoons as much.”
The lingering question, both about Gruber’s Sleep for Success curriculum and Eastern Commerce’s 10 a.m. start, is a simple one: Why do these inexpensive, eminently sensible ideas remain isolated experiments? No doubt inertia plays a part, but there’s more to it than that. When Gail Somerville applied for more funding for Sleep for Success, she was denied, because Quebec’s education ministry preferred to start a careers program for young children. No one seems to have considered the idea that sleep can be crucial for successful careers.
Still, the Riverside School Board and Eastern Commerce initiatives signal that the pendulum is beginning to swing—that we may yet become a more sleep-savvy culture. Since 2011, SickKids has put on a biennial pediatric sleep symposium that sells out quickly and creates awareness among health care workers. In Vancouver, Osman Ipsiroglu, along with a group of parent advocates, co-founded the Children’s Sleep Network, an information resource for health professionals and families.
Every once in a while, interest in the subject surfaces in unexpected places. Last fall, Ipsiroglu was contacted by a First Nations band in the Maritimes. Worried that their children were not dreaming, the band invited him to speak in the fall of 2015. “This is a tremendous observation,” Ipsiroglu says, “because if you don’t dream, your sleep architecture is disturbed. And that is what concerned them.”
And then there’s Fatigue Science. The small Vancouver company—which doubled its business in 2014—counsels twenty-five sports teams, including the Seattle Seahawks, Vancouver Canucks, and Toronto Raptors, showing them how athletes can cope with games in different time zones. Rest, they tell them, is key to performance. Sam Ramsden, the Seahawks’ director of player health and performance, cites the fictional assassin Jason Bourne as an inspiration. “Bourne’s goal was to get more sleep than his enemies,” Ramsden says. “We’re teaching our players: sleep is a weapon.”
This appeared in the May 2015 issue.





