What goes into a Nanaimo bar? Answer: a Hells Angel, a bouncer, and a drug dealer. It’s an old and mostly obsolete joke but, in the way of jokes, it captures, or once captured, a truth. In the ’90s, the Hells Angels gang was highly visible in this mid-sized Vancouver Island city; when the resource economy was in decline, many loggers, fishers, shipwrights, and mill workers were idled, but the bars weren’t; in 1994, the Washington Post wrote about Nanaimo being named “Canada’s heroin capital.”
At the time, a miner’s cottage, the local term for a small home with practical aesthetics, could be had for $60,000—likely less if the roof leaked. Cedar shingles last about thirty years before they go soft. The last of the bustling coal mines closed in 1986. A lot of the roofs leaked. As many as 42.6 percent of single people lived below the poverty line in 1995.
This was thirty years ago. The province of British Columbia seized some of the Hells Angels clubhouses. Unemployment peaked at 12.5 percent in 2001; now it is 3.6 percent. All around the core: expansive developments of recently built homes. Taken as a whole, the community has nicely emerged into a post–resource extraction economy. Most of the new houses are roofed with asphalt shingles now, wood no longer being essentially free, and there are a lot of metal roofs too. The cladding of the houses is often Hardie board—imitation wood made of painted cement. Little risk of rot. The shiny homes are themselves a sort of cladding. What they envelop in the centre of Nanaimo is, as it is in cities across North America, a public health crisis and the defining moral failure of our era.
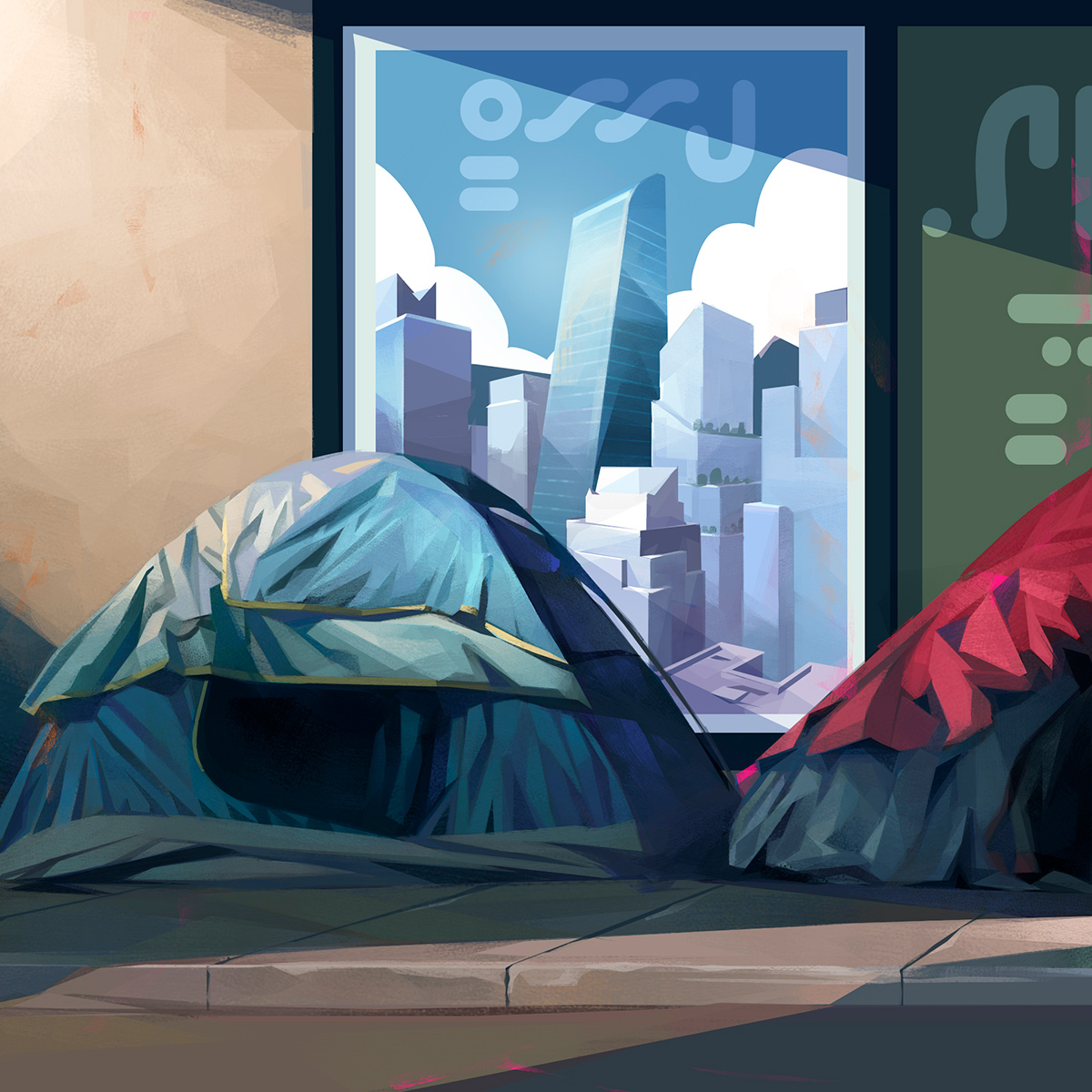
Even as unemployment has fallen and mean income risen, in the centre of the city, there is a more visible and abject agony than was seen when unemployment was four times as high. There, people stagger and weep and sleep in doorways and are quickly coming to define this neighbourhood—just as the Downtown East Side in Vancouver has long been so defined. Brightly coloured dome tents have appeared in vacant lots and, for as long as they are permitted, in parks. For nearly a year, the approximately 300 people of Discontent City, as it was called, lived beside the ferry terminal to Gabriola Island. The encampment was dispersed in 2018. There had been tent fires and violence.
The number of unhoused in Nanaimo has since grown—by 2020, a 29 percent increase from two years before. Since then, with the COVID-19 pandemic, much more than that. Officially, there are around 650 unhoused people in a city of just over 100,000, but the precise number is hard to know. City councillor Erin Hemmens told Nanaimo News Now, “A lot of those folks are hiding in bushes, a lot of those folks are not facing active addiction. A lot of those folks are trying their best to avoid detection and they include seniors, families, they include youth and single women.” Whatever the total number is, it is growing fast, and the human beings who comprise it are changing all the time. People arrive on the street and then depart it. When COVID-19 surged and house prices and rents spiked, that gust shook loose a lot of people whose grip had already been tenuous.
When winter rain comes, human beings gather under overhangs and awnings to sit on cardboard or on rolled sleeping bags. It’s the Pacific coast. Everything gets damp. The cold of the sidewalk seeps up even through boot soles. And so human beings huddle to provide one another warmth and solace. Their faces announce how much time they spend outdoors. Many of these human beings look two decades older at first glance than they do up close. They form small circles, facing one another. Sometimes they do drugs. Sometimes someone sleeps beside them. Sometimes that person doesn’t wake up.
Tents catch the eye, but what the public mostly doesn’t see is what emergency medical technicians do every day, all day: respond to a constant dirge of overdose calls. There were more than 33,000 overdose calls in British Columbia last year; there were 1,455 overdose deaths in the first seven months of 2023, on pace to exceed the 2,383 last year. Among children aged ten to eighteen, overdose from opiates and other illicit drugs is the leading cause of death in the province. Across Canada, an average of twenty people died of that cause every day last year. In the United States: nearly 107,000 dead in 2021, according to the Centers for Disease Control and Prevention, more than double of the figure for deaths due to guns. The COVID-19 pandemic caused a surge in overdose deaths across North America. Isolation. Loneliness. The severing of supports.
COVID-19 death rates have settled. Drug overdose deaths haven’t. To the physicians and nurses in ICUs and ERs, this wave of deaths seems inexplicable and horrifying. The numbers are discussed often in the media, and compassion fatigue has set in: a May 2023 op-ed in the Globe and Mail was headlined “The Public Is Fed Up with Open Drug Use in Parks and Downtown Cores.”
Set aside the why for a moment and contemplate the what: corpse after corpse, once beautiful human beings, found cold and stiff in the streets in the rain or the snow, or on couches in the aftermath of parties, or slumped in chairs in apartments and homes. Some in sleek hotels and condos. More than two-thirds of them men. A large portion of them alone. Some high school students. Some after snorting what they thought was cocaine for the first time. Some had smoked what they thought was only weed.
Fentanyl can be present in any drug one might buy away from the light. According to a 2020 report from the Canadian Centre on Substance Use and Addiction, 10 percent of BC’s methamphetamine samples and 7 percent of its cocaine samples contained fentanyl. Synthetic opioids have made drug use more lethal. Most of the illicit fentanyl comes from Mexico and China. It is cheaper than heroin and has largely displaced poppy-derived narcotics on the street. Fentanyl isn’t intrinsically more dangerous than other narcotics; in the hospital, in known concentrations, it is used regularly for analgesia and sedation. It causes slightly less hypotension in equivalent dosages than other narcotics do, and it acts and wears off more quickly than morphine or hydromorphone.
The rapid onset and wearing off make it safer to use in the hospital but also more addictive. Tobacco companies have known about this theory for decades, adding adulterant chemicals—accelerants—to tobacco to produce a similar result with nicotine: increasing the chance of addiction. But no user really knows just what they’re taking anymore.
The mixology of narcotics drives much of the toxicity. Levamisole, a veterinarian deworming agent, is sometimes mixed in with fentanyl. It can induce a profound suppression of the bone marrow, causing neutropenia, or low white blood cell counts, which renders patients susceptible to infections in the same way that chemotherapy patients can be. Recently, benzodiazepines—Valium-like drugs—have become commonly used adulterants. This matters because naloxone, brand name Narcan—the safe and dramatically effective opiate antagonist—does not reverse benzodiazepine-induced unconsciousness.
This year, there has been a surge in toxic drug deaths in Nanaimo. People coming to the hospital with overdoses acted differently than people with pure narcotic overdoses usually do. They were agitated rather than somnolent and frequently had seizures. This constellation of symptoms is called a neuroexcitatory toxidrome and is more characteristic of cocaine or amphetamine overdoses. But in many of these patients, the only drug found in their urine was fentanyl. It seems likely that something else was there that isn’t understood—and isn’t yet being tested for.
Whatever adulterant it turns out to be, it seems likely that it is related to the recent surge in mortality. Why not cut fentanyl with something more benign like corn starch? Baking soda? Talc? Maybe the drug cooks are inspired by the tobacco companies. They have something of the same ruthlessness.
A prevalent narrative asserts that this—the tents, the despair, the not waking up—is about undertreated mental illness wound around its cause and consequence: addiction. It’s a comforting tale for the inner puritan, but that narrative crumbles after the first questions.
Why would disabling mental illness be so much more common now than in the 1990s? Why are there so many more homeless people now? The unemployment level is at near-historical lows, continent wide. Violent crime is a fraction of what it was in the 1990s. The stock markets are within 10 percent of their all-time highs. There hasn’t been a recession not mediated by a virus in a decade and a half. Is this not, at least by census data, an easier and more prosperous time than any before?
Homelessness, addiction, and mental illness are not the same thing. Most of the unhoused are not addicted. Many overdose deaths are among housed people, and about a quarter in people who are unhoused. So with the other combinations. These three do not equate; they don’t always have the same cause. But they’re related. Homelessness, addiction, and mental illness occur frequently in similar populations, and they keep one another’s company. When doctors find one of these, they look around for the other two. A medical lens, trained on the tents and the dead, observes a similar agglutination. It is as if eviction notices change people.
The average price of a single-family detached house sold in February 2023 in Nanaimo was more than $700,000. That’s about fifteen years of average pre-tax earnings. The average rent is pushing $2,000 per month. Especially in extreme-winter countries, shelter is as necessary as food, and its want proceeds to the same conclusion. On a daily basis. In some cities in Canada, the median age of death among the unhoused is nearly half that for the general population.
In North America, the indifference, even hostility, of government, the market, and voters to the unhoused population is evident at a glance. The tents exist because Canada doesn’t have enough housing. (To restore housing affordability, the country needs an additional 3.5 million new homes by 2030.) When Nanaimo’s miner’s cottages were built, they were built small and on low budgets and often by the homeowners themselves. Through the last two decades of the twentieth century, all over the country, housing prices increased slowly and steadily, at about the same rate as inflation—in constant dollars, house prices remained constant. Since 2010, house prices in cities, including Toronto and Vancouver, have doubled. Productivity gains and low interest rates—an era economists call the Great Moderation—fuelled an economic expansion beginning in the mid-’80s that has continued, with some comparatively brief interruptions and pauses, to this day. Huge amounts of wealth were generated by Western economies in the years that have followed, and much of that has been ploughed into real estate—especially housing. House prices and rents ballooned and have yet to pop in the way pets.com did.
Homeowners—disproportionately older and richer and more likely to vote—have been gratified by the spiking value of their homes. In Canada, the capital gains exemption for principal dwellings meant the country lost $5 billion in tax revenue in 2017. In America, the mortgage interest deduction amounts to the same sort of subsidy—roughly $190 billion (US), almost quadruple of what is spent on direct housing assistance to the needy—for the rich. Among many families, selling the home has become an entirely viable retirement plan. But surging house prices and interest rates make for surging rents—by driving would-be buyers to rent instead and increasing demand, and by changing how much rent landlords must charge to cover their own mortgages. Average rents exceed what can be paid on a minimum-wage income—or even considerably more than that. Many people have no options.
Current homeowners benefit from the shortage of housing because it propels further appreciation. Apartment blocks are resisted; social housing is anathema. Many people who own real estate want little else built—no matter the damage done to the vulnerable and to their own community.
Every $100 (US) increase in average rent increases homelessness by 9 percent, according to a 2020 report by the US Government Accountability Office. Even among the housed poor, the burden of rent can be suffocating. It is a choice—NIMBYISM in the small scale and a streak of puritanic meanness within us in the large—that some people must sleep in tents. Nobody disdains the failing more than the recently successful. Virtually every homeowner has become wealthy in recent years. Kitchen counters used to be formica. Now they are granite, the pink flecks of feldspar within echoing the brightly coloured tents of increasingly grey downtowns.
Medicine is an intensely pragmatic discipline: it is to biology what mechanical engineering is to physics. Outcomes trump every theory; for many of its most effective tools, the understanding of how they work is either incomplete or absent entirely. Equally incomplete is a medical explanation for the startling pan-continental rise in deaths due to suicide, alcoholic liver disease, and drug—especially opiate—overdose since the turn of the century. In 2015, these were branded “Diseases of Despair” by Anne Case and Angus Deaton, writing in Proceedings of the National Academy of Sciences. Deaths due to them doubled in America between 2009 and 2018. First recognized epidemiologically as a flattening and then as a decline of life expectancy, especially among middle-aged, non-college-educated white men, the phenomenon gained international attention with the OxyContin crisis. In the manner of epidemics, the crisis spread—at first, slowly—across North America.
“Despair” is not a word doctors usually use. If they must discuss unhappiness, as in depression, they are more likely to use drier words like “dysphoria” or “anhedonia.” Despair is an amorphous idea, and the word exists in the vernacular, denoting a collapse of hope and faith. It has emotional content reflecting exactly what it describes.
Through the twentieth century, life expectancy in North America lengthened by 2.5 years per decade—extraordinarily fast. Diseases of poverty, such as tuberculosis and measles, receded as average income and health care improved. The diseases of despair are posited by Case and Deaton to be different from those of poverty, occurring not in the poorest circumstances but in the most hopeless. They correlate highly with inequality and dispossession. Generational declines in well-being are especially apt to summon them. The industrial economy collapsed in the Rust Belt of the continent earliest and hardest, but the fishers and loggers in the bars in late-’90s Nanaimo were an expression of the same process.
As elsewhere, a lot of people have done well, and the GDP has grown. But homelessness has grown in step. Rising tides do not float all boats—literally or metaphorically. Fishers tell stories about the tenacity of the muck of tidal flats and the way it sometimes holds boats in the mud until the sea rises to the gunwales and then there is no longer any holding down of anything to be done. Rising tides are fine if you’re already buoyant.
Vancouver island is about 460 kilometres long. In its centre, there are glaciers and the sort of deep and cold lakes that mountains and ice make. Running as a kind of fringe around the inside and outside coasts of the island is temperate rainforest: red cedar and Douglas fir, mostly. On the inside passage, the humpback whale population is growing, after a forty-year low. This a lush place; at a ten-minute walk into the forest is stillness.
But we live in communities built where the forest has been razed, where stillness and tranquility are now mostly abstractions. The least distressed of Vancouver Islanders are, inevitably, the richest, and they live in Victoria, the provincial capital, where decisions about the allocation of health resources, including mental health resources, are made. Life expectancies decline the further away from a city one goes, and communities at the disadvantaged end of this gradient argue for a redistribution of health care resources. Those making the decisions, those with voices in this discussion, are generally the rich who live in Victoria, inconveniently far from their brethren. It is only partly a matter of geography. It’s mostly about income.
At the very end of our lives, when our last hours are more likely to be occupied with cancer or heart disease, we have multi-million-dollar supports, like the Peter Munk Cardiac Centre in Toronto or the University of Ottawa Heart Institute. But the thing that makes the biggest dent in us before then is despair. The size of the dent is, on average, smaller among the rich. The experience of the poor is different.
There is growing evidence that the lifetime risk of depression is inversely related—more strongly than any other health outcome—to income and education. The neglect and underfunding of mental health are constantly apparent in an ICU. Were it not for the diseases of despair, a large portion of the beds would be empty.
As with cedar shingles: enough cold rain for long enough and humans soften too.
There is a superstition about problems coming in threes. In medicine, triads are trouble. The lethal triad of trauma is acidosis, hypothermia, and inability to clot. The diseases of despair also appear as a triad: suicidal ideation, drug overdose, and alcoholic liver disease. And the organizing pathology—the root—of despair is inequality-related homelessness, just as gallstones are to cholangitis and bleeding is to trauma shock. Each of these sends patients to the hospital regularly.
In the hospital, socioeconomic class does not announce itself as loudly as it does outside it. Patients all wear the same gowns. Expensive jewellery is sent home with relatives. Everyone is washed and, if they want it, shaved. In the ICU, patients on ventilators are usually sedated; the preoccupations of medical staff become the immediacies of blood pressure and oxygen. Mood is hard to discern in intubated patients. The nature of one’s domicile, be it oceanfront home or tent, is not often discussed.
Everyone is marked by how they have lived. As we are all marked by how we have treated others.





