Michael Riddell’s lab is a diabetic’s paradise. The large white room at Toronto’s York University is dotted with treadmills and transmitters; there are tiny blood-testing strips, insulin-pump infusion sets, and hot-peach bottles of glucose tablets galore. I’ve come here, alongside a half-dozen innovators and keeners in the diabetes world, because it’s said to be ground zero for a technological revolution. All of us are either diabetics or the parents of diabetic children and, as such, are equally obsessed with finding better ways to live with the disease. We munch on sugar-free cookies and sip diet cola, but when Riddell starts to describe the work he’s doing, we stop and listen as though our lives are on the line. Because, really, they are.
Listen to an audio version of this story
For more Walrus audio, subscribe to AMI-audio podcasts on iTunes.
Diabetes is a tricky disease, both to live with and to understand. It all comes down to the pancreas: in normal circumstances, the organ produces insulin, a hormone that controls blood glucose. Diabetics either can’t produce enough insulin (which causes the more manageable type-two diabetes) or any at all (type one), so our bodies can’t properly deal with the sugar we consume. When blood-glucose levels drop too low or surge too high, it can lead to serious health complications. One hundred years ago, children all around the world would slip into comas and die because of type-one diabetes. Then came Frederick Banting, who led the team that, working out of a University of Toronto lab in 1921, discovered insulin. He extracted insulin from animals and injected it into terminal comatose patients. Like little Lazaruses, the children came back to life. Banting’s work has since been hailed as one of the great medical achievements of the twentieth century and has allowed type-one diabetics—myself included—the opportunity to live full, relatively normal lives.
Managing type one, however, is a full-time job—one where, if you don’t do it just right, you’ll feel terrible. Or get sick. People today still fall into comas because of diabetes. People today still die. And, though treatment has improved over the decades, the reality of living with the disease today isn’t so different from living with it in 1921: diabetics must decide how much insulin to take when their blood glucose goes high, and how much sugar to consume when their blood glucose goes low, to try to get their levels as close to a non-diabetic’s as possible.
The magic number for blood glucose is typically 5.0 millimoles per litre, and consistently hitting it is a challenge, even for those with the most up-to-date medical technology. There are insulin pumps that allow people with diabetes to forgo regular insulin injections: these devices, which look like pagers, hook onto belt loops and run a thin tube through a tiny hole in the abdomen to deliver a programmable stream of medication. There are also continuous glucose monitors (CGMs), sensors placed under the skin that can replace the old prick-and-drop test strips by sending updated blood-glucose levels to users’ phones every five minutes. But diabetics still need to consider many factors and make many calculations to determine how much insulin they need to take: what they’ve eaten (and what they’re going to eat); how much exercise they’ve done (and whether they’ll exert themselves in the coming hours). Stress, hormones, illness, sex, weather—all can affect blood sugar. The trick is to think like a pancreas. The problem is that nobody really understands how a pancreas thinks.
This is where Riddell’s research comes into play. His work seems personal: he’s been living with type-one diabetes for thirty-five years and is the father of a teenage son who lives with the same disease. Riddell and his colleagues are working with Google’s parent company’s health offshoot, Verily Life Sciences, to study an activity monitor that can check blood-sugar levels during exercise. “We’re hoping everyone will be able to afford this in the not-too-distant future,” he says. “Paired with an artificial pancreas, it will be incredibly precise.”
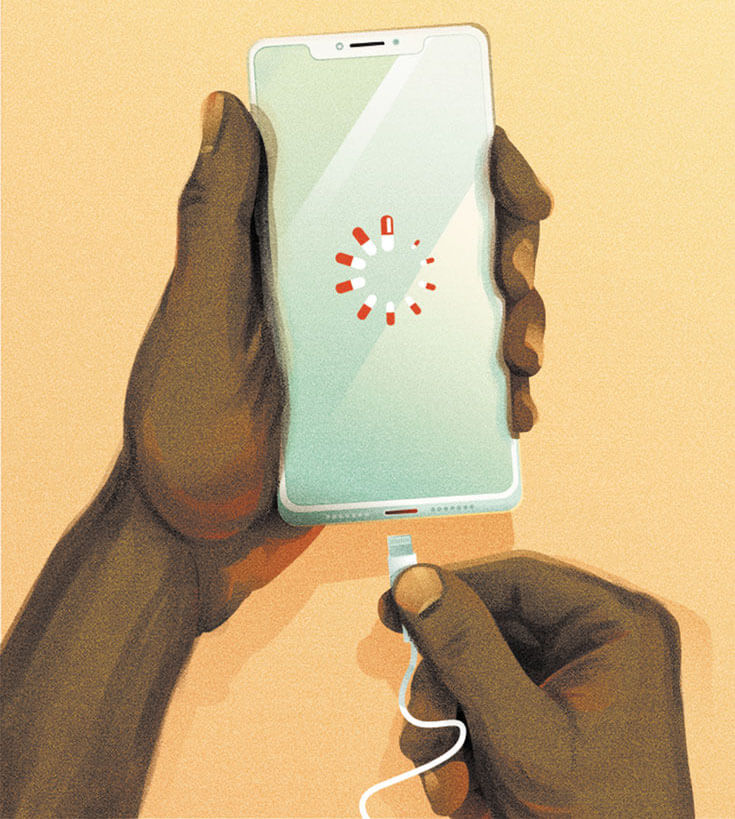
“Artificial pancreas” isn’t a term I’d heard before. I ask Riddell to explain. “So, you have your insulin pump and your continuous glucose monitor,” he says. “Great technology. But these devices don’t talk to each other. You’re the one who’s still making the decisions. You have to interpret the numbers, analyze the trends, predict what you’ll be doing later in the day, and figure out how much insulin to take. What if a computer could do that for you?”
Riddell explains that most major medical-device companies are now gunning for this kind of call-and-response system, where an insulin pump communicates with a CGM in real time to automatically adjust insulin according to fluctuations in blood-sugar levels. This is the artificial pancreas, also known as “the closed loop,” and it’s the holy grail of diabetes management. Ideally, the closed loop takes all the complicated decision making out of the hands of the patient and simply works in the background like any other organ.
As a lifelong diabetic, this kind of technology sounds like the stuff of science fiction. I ask Riddell how long it’ll be before an artificial pancreas actually becomes available. “Well, officially,” he says, “probably a few years. The challenge in all of this is getting federal approval, of course. Clinical trials can take years and cost millions of dollars. But, unofficially—”
Riddell gets cut off by one of the attendees beside me. “My daughter’s on it,” says a woman named Kate Farnsworth. “Mine too,” adds Pina Barbieri.
Having lived through decades of glacial advancements in diabetes technology, I’m incredulous. Health care devices are notoriously slow to update and improve—my insulin pump feels a decade behind the customization and adaptability found in my iPhone—and what these women are describing is an incredible leap in treatment. But Farnsworth insists that it’s true.
She explains that, a few years ago, a group of amateur coders, most of them type one themselves, were independently fiddling around with insulin pumps and CGM transmitters on their off hours, looking for ways to improve the devices. They eventually met, pooled their discoveries, and after a few more years of tinkering, created an iPhone program called Loop. It’s not available in the App Store or through any official channels—no doctors will prescribe it. Users need to find the instructions online and build the Loop app themselves. This bit of free code, Farnsworth tells me, paired with a hacked-together insulin pump and CGM, is an artificial pancreas.
“Is this legal?” I ask, imagining some dark alley where hooded hackers hand out instructions and tiny radios to desperate diabetics.
“Of course,” Farnsworth says, laughing. “It’s open-source software. It’s also a Facebook group. You can find everything you need online.”
“Are you on this Loop?” I ask Riddell.
“No, but I’d like to try it,” he says. “I mean, why not? Kate, want to host a build party for Jonathan and me?”
“Sure!” she responds.
I laugh nervously. I don’t tell the group that I feel uneasy about entrusting my life to some homemade software thrown together by amateurs. What if the algorithm is off and my phone, instead of calling my mother, decides to give me 300 units of insulin, sending me into diabetic shock? The technology sounds revolutionary—if it actually works—but it also feels like giving up control. It’s taken me thirty-three years to gain even a small amount of power over diabetes; I have trouble believing that a few lines of code can actually understand my body better than I can.
Iwas twelve when my immune system suddenly wiped out the insulin-producing beta cells in my pancreas. I was in Paris on a family vacation at the time, and the first symptom arrived when I started urinating like crazy, drinking litres of water each day to compensate. My memory of the Champs-Élysées is not the beauty of the architecture but the number of public bathrooms I had to duck into along the way, pissing accumulated sugar like a human glucose siphon.
Insulin is a life-sustaining hormone, taking food that’s been broken down into glucose and transporting it to cells as energy. Without insulin, we wither away. I was told all this a little later during that same trip, shortly after we traded the streets of Paris for a London hospital room. It was 1986, a different era in diabetes care, and the doctors told me I could still eat whatever I wanted, so long as I injected enough insulin to compensate for the carbs consumed (advice that would prove to be technically true). I was told that diabetes is manageable, that you can live a good life with it—both correct—but my diagnosis still changed how I saw myself. I contained a flaw, my body now a series of problems that constantly had to be re-solved.
A nondiabetic’s blood-glucose level stays relatively stable around 5.0 millimoles per litre. I soon discovered that mine could jump from 2.6 to 21.5 in a day. (It wouldn’t be a good day, mind you.) This was the time of test strips where you dropped blood, wiped, and waited for the colour to change: green was good, brown-green higher, red too high. I’d read my results, draw back on my insulin needle, and plunge.
I was informed that these swings in blood sugar could potentially lead to serious health problems. If I took too little insulin and my blood sugar went high, I worried about ketoacidosis, which can trigger a diabetic coma, as well as long-term complications including blindness, kidney failure, and neuropathy. When I took too much insulin, my blood-sugar dipped low, giving me mind-blowing munchies, as well as thoughts about how I was risking coma and death. Banting’s discovery of insulin was not a cure, and figuring out the right amount of insulin to take involves sleuthing, scientific interpretation, and constant self-monitoring. As a teenager, I was shooting in the dark, trying to hit that perfect 5.0. It’s a lot of work under the best conditions, and besides, I was a kid—I wanted to have a life.
Ten years ago, after over two decades of injections, I got an insulin pump, a newer device that changed my life. When injecting insulin, I often felt exhausted and generally unhealthy. I’d previously made lifestyle changes to try to get my blood sugar under control—I quit booze, started a low-carb diet, and exercised religiously—but found it was the constant flow of insulin through the pump that made all the difference. And, though I became ruled by the pump (one can’t disconnect for longer than an hour), it was worth it. My energy levels improved, and I started doing triathlons, long-distance swims in open water, and cross-country skiing. My blood-sugar control also became better, which means a potentially longer life with fewer complications.
Even though insulin pumps have clear benefits, they are still uncommon. There are approximately 300,000 people in Canada living with type-one diabetes, and most reports peg the number of these people with pumps at less than 40 percent. Many are reluctant to switch because pumps are expensive (around $7,000) and aren’t covered in some provinces. They also come with a steep learning curve, and properly programming them can be difficult for those used to the simplicity of injections. And, even with the technological help, there is still an element of guesswork involved: I can weigh my food on a scale, dial in exactly the amount of insulin that my diabetes team and I have determined necessary, and my blood glucose can still take off for unknown reasons—maybe it’s the end of a bottle of insulin, or a kinked infusion set, or just a bad day.
The fact that so much can go wrong is frightening, and I’m not alone in feeling this way. In Riddell’s lab, I speak with Farnsworth, who’s in her early forties, about the fear she felt when her then eight-year-old daughter, Sydney, was diagnosed in 2012. “I looked everywhere for information,” Farnsworth says. She describes researching all the promises offered by medical companies, hoping that some piece of technology would make managing the disease easier.
The first device that got her hopes up was the Dexcom G4 CGM, which uses a sensor to continuously check blood-sugar levels. In theory, this would tell Farnsworth whenever Sydney’s blood glucose was high or low. But Farnsworth quickly discovered that the device was only available in the United States—Health Canada hadn’t yet approved it. She fought her doctor to get a G4 and eventually won. (It finally became available countrywide in 2013.) “I thought, ‘Awesome, this is going to solve a lot of problems,’” Farnsworth says. “But it didn’t fix everything. For starters, we didn’t have access to the information—only Sydney did.”
The G4 had limitations that felt archaic in the smartphone era. Users could read blood-glucose levels only on a specific Dexcom-brand receiver—one that worked just up to twenty feet away from the patient without obstruction. This meant that, even when she and Sydney were at home, Farnsworth could have difficulty reading her daughter’s levels.
These limitations became especially evident at night. Getting a proper sleep may be the single biggest challenge for people with type one, as a night with low blood glucose is disorienting and life-threatening. The problem is existential: If my levels drop, will I wake up in time? Before getting the G4, Farnsworth used to set three alarms throughout the night so she could wake up and prick Sydney’s finger to make sure she wasn’t falling too low. She found that, even with the G4, she’d have to wake up and get beside her daughter to check on her.
In May 2014, Farnsworth came across a blog post in which a parent of a child with diabetes mentioned offhand that they had managed to connect a CGM to a cellphone. Farnsworth was amazed that this was possible, and she was led to a Facebook group called CGM in the Cloud, an international community of 30,000 members with a do-it-yourself ethos, all of whom were interested in hacking existing devices to find new ways to manage the disease. Like Farnsworth, members felt that official health channels, with their long regulatory delays, weren’t always working in the best interests of diabetics. They created a hashtag to rally around: #WeAreNotWaiting.
Through the Facebook group, Farnsworth followed a set of instructions offering an open-source hack for Sydney’s G4. Suddenly, thanks to this free code and help from community members, she was able to pair Sydney’s CGM with a regular Pebble smartwatch, giving her the ability to check Sydney’s blood-glucose numbers wherever she was. She was even able to set up an automatic alarm to warn her whenever Sydney’s levels were trending low.
After Farnsworth gained the ability to read Sydney’s blood sugar remotely, she started wondering how she could get enough control over the disease to prevent the night lows from happening in the first place. In 2016, Farnsworth attended a Children with Diabetes conference in Anaheim, California, where she heard one of the participants talk about Loop. It was the DIY artificial pancreas. She knew that Sydney had to have it.
Loop is not a specific device or a ready-made product. Essentially, it’s some lines of computer code that can turn a traditional insulin pump and CGM into an artificial pancreas. Its roots go back to San Francisco in 2010, when Ben West, a software engineer and type-one diabetic, spent several years’ worth of his evenings and weekends finding a way to remotely control his Medtronic insulin pump by exploiting a security flaw. Meanwhile, type-one diabetic Dana Lewis and network engineer Scott Leibrand were in Seattle, at work on an algorithm that could predict blood-glucose levels in response to trends compiled by a CGM. The three eventually found one another at a conference, shared their knowledge, and in doing so, created the first DIY artificial pancreas. Lewis and West tested it on themselves and posted their results and the instructions online. Other developers, including Nate Racklyeft and Pete Schwamb, also set out to build a system around Ben West’s discoveries, and in 2015, created their own insulin dosing algorithm that ran as an iPhone app. This app, which had an easy-to-use interface, was named “Loop,” and a movement was born.
“When Sydney started on Loop, my entire role as a parent changed. It went from me micromanaging her diabetes to the system doing almost everything,” Farnsworth tells me. She no longer needed to wake up in the night worrying about Sydney going low—Loop took care of that by reducing Sydney’s insulin whenever her blood sugar began to dip. Farnsworth notes that Loop isn’t perfect—the user still has to input the carbs they eat and can include the exercise they get—but it has made a remarkable difference in their lives. “Now that we’ve got the hang of it, every night she goes to bed, I sleep through the night, and she wakes up at the same number,” she says. “It’s amazing.”
“Yeah, she actually gets some sleep,” says Pina Barbieri.
Suddenly, an alarm goes off. It’s Barbieri’s Pebble watch. Her daughter Laura’s blood sugar is 17.3, which is very high. Barbieri texts her: “You okay?”
Laura: “Yeah, taking more insulin.”
Barbieri: “Good.”
This exchange between mother and daughter floors me. I’ve always felt that there’s something intimate about blood sugar: shame if you’re too high; pride in perfect fives or sixes; anxiety if you go too low. It’s like having a daily report card on how you’re living your life. When I was thirteen, my father would ask me how my blood sugar was, but he didn’t pore over my logbooks and analyze their trends; my mother weighed my carbohydrates on a scale and cooked meals without sugar, but in the end, managing the disease was down to me, and I’d tell myself that I needed the privacy. I’ve never even shared my numbers with anyone other than my doctor. As I listen to Farnsworth and Barbieri, I wonder if I’ve been thinking about diabetes all wrong.
Ispend the next few months reading posts in the Looped Facebook group, which, at the time I join, has about 6,500 members from all over the world. Approximately 1,000 of them are “Looping” and come to the online community for practical tips and troubleshooting advice. Others, like me, are curious for more information. Everyone seems supportive, generous, and kind, which feels like a social-media miracle.
As I fall deeper into this online world, it becomes clear that the type-one community has been helped by the internet in ways that were unimaginable when I was a child. I wonder what kind of tips I might have picked up had I had such forums instead of relying on my twice-yearly visits to the endocrinologist’s office, which lasted all of ten minutes.
The more I learn about Loop, though, the more hesitant I feel. For one thing, Loop requires having a hackable pump, and I discover that these are rare: when medical-device developer Medtronic realized there was a security flaw in its products, it changed its design to close this back door—its official concern was that hackers could remotely dose a user with a life-threatening amount of insulin. This change makes Looping with new pumps impossible, meaning would-be Loopers need to find old, out-of-warranty Medtronic devices. They also need to order a RileyLink from the United States— this small Bluetooth device is what lets an iPhone communicate with a pump. After all of that, they need to build the Loop app themselves. Making the switch from injecting to the pump was enough work; this feels like too much effort for an unproven payoff.
Still, I continue to correspond with Barbieri and Farnsworth. Farnsworth explains that, since Loop has given her and Sydney so much, she feels compelled to give back to the community: she’s the creator of the Looped Facebook group and is one of the two volunteers who run the page, spending hours each week answering questions and offering advice. She even sets up a FaceTime conversation between me and Sydney so I can ask her if the DIY app is as good as everyone says. “Loop is as close to perfect as you can get,” Sydney replies.
Then Farnsworth mentions something that surprises me: “At one point, she said she wouldn’t be the first in line for the cure.” Sydney goes on to explain that there are gifts she’s gotten from diabetes that she wouldn’t want to trade, like her friends at diabetes summer camp. I’m startled because, for me, diabetes has always been a daily gauntlet of decisions, something I associate with the constant stress of staying alive. When I was Sydney’s age, I even kept my diagnosis a secret from my classmates, ducking into the bathroom to discreetly inject myself and quietly popping orange dextrose tablets as if they were cough drops.
One day, not long after this conversation, Pina Barbieri calls to say that she and Farnsworth would like to organize a Loop-building session with Riddell, myself, and a few others. Barbieri has an old, Loop-able pump that I’m free to use, and she says she’ll also give me her daughter’s extra RileyLink so long as I replace it. The entire cost of this life-changing artificial pancreas? $250. Amazed by the generosity of a virtual stranger, I thank her. But, when she asks me to commit to a date, I’m evasive. I’m still not sure if I want to be a human guinea pig in the diabetes revolution.
Days pass, and the dream of the closed loop clings to my imagination. I call Health Canada and am put in touch with Graham Ladner, scientific evaluator of the medical-devices bureau. I ask him about the elusive artificial pancreas. I want to know how far we are from seeing an approved version on the market.
Ladner explains that an insulin pump is usually a class-three medical device, but once you “close the loop” by having the pump automatically communicate with a CGM, it becomes class four, meaning more restrictions and more difficulty getting approval. Ladner tells me that closing the loop is a big challenge for Health Canada because so much can go wrong, particularly in the over-delivery scenario.
That makes sense: if my CGM erroneously says I have a blood glucose level of 16.5, but I’m actually at 7, the pump will automatically give me too much insulin and I’ll end up with severe low blood sugar and possibly lose consciousness. This heightened risk is no small thing—even in normal use, insulin pumps can be dangerous. According to an investigation published by the CBC in November 2018, more people have died because of insulin pumps than any other medical device on the market, with Health Canada concluding that they may have been a factor in 103 deaths and over 1,900 injuries from 2008 to 2018.
Ladner goes on to tell me that CGMs have been known to send incorrect blood-glucose measurements. “The [closed-loop] system relies on their accuracy. That risk exists now, with pumps, if you take insulin based on your CGM reading. But it becomes magnified when you let computer algorithms calculate things,” he says. “The closing of the loop introduces new patient hazards, and we need to be convinced that it’s safe.”
When I mention the DIY Loop app making the rounds online, he says he doesn’t know much about it. “Is this illegal?” I ask. “No one is making any money off this, so we can’t really say or do anything,” Ladner says. “But remember, CGMs aren’t perfect.”
After I hang up the phone, I head back to the Looped Facebook group. I’m not sure what I’m looking for—confirmation? A perfect solution? I read a concerned mother’s comment about some of her frustrations managing her child’s diabetes: a brilliant rant about the injustices of the universe. Fellow Loopers chime in with choruses of support and advice. I choke up, break down, and cry. Maybe it’s the exhaustion of living with diabetes for thirty-three years. Chronic illness affects us in ways we’re often not aware of.
I have cried only once before because of my disease. It was my second day in that London hospital, and I was learning how to inject insulin by practising on an orange. It was the moment I understood that diabetes is a life sentence. My mother was outside my hospital room, and at first, I wasn’t sure what she was doing alone in the hallway. It was the first time I saw her break down too.
As I read the various Facebook comments, I’m amazed by the care people take in volunteering their time, feedback, and insights. Which is why I decide to do it. Will the Loop be better than what I have? I don’t know. But, for the first time, I won’t have to do it alone.
It’s a Saturday morning when we meet again, back at Riddell’s lab. Riddell, Barbieri, Farnsworth, and I are joined there by Dana and Marley Greenberg, mother and daughter, ages fifty-two and nineteen, both type one. The mood is festive as Barbieri brings out gluten-free donuts and crullers. Farnsworth hands me an old purple Medtronic 554 pump, a rare commodity. Barbieri passes a white box the size of a lighter: the RileyLink. Once connected, these two devices will work alongside my CGM and the Loop code to create my artificial pancreas.
Dana Greenberg tells me she has been diabetic for forty-four years, a lifer like Riddell and me. She asks if she can help insert my CGM sensor and transmitter on my arm, a spot I can’t easily reach. I nod and she swipes the back of my forearm with an alcohol swab, fans it dry, then slaps the needle inside me.
We gather at a lab table with our phones and laptops. Farnsworth leads us through all the steps of inputting the computer code. A message appears on my screen: “Please understand this project is highly experimental and not approved for therapy. You take full responsibility for building and running this system and do so at your own risk.” I continue on.
By the end of the afternoon, I’ve built my first app and transferred it onto my phone. We connect finicky wiring to tiny battery packs and flick on our RileyLink switches. When I tap the Loop icon, I see graphs highlighting my glucose trends, active insulin, insulin delivery time, and carbohydrate intake. My CGM numbers appear on the top row. To the right, it shows how much insulin the algorithm is adjusting. To the left, a small circle glows green. The green means I’m looping. My artificial pancreas is alive.
In the days that follow, Barbieri and Farnsworth continue to guide our group through instructions and problem solving via group chat. At first, I feel overwhelmed and am constantly worried I’m going to forget something—there are so many moving parts. Sometimes the RileyLink craps out and the Bluetooth goes down, and I feel panic in the moments before it reconnects. There’s no question that the system isn’t perfect. But, after my first night’s sleep, I wake up to a perfect blood glucose of 5.0. And then it happens the next morning. And the next.
A few days later, my insulin pump blanks out: the screen disappears. I try a new battery, but it doesn’t come back on. In a panic, I immediately write to the group: “Does anyone have an extra pump?”
“You might want to consider looking on Facebook or Kijiji for a backup,” Dana suggests.
Riddell joins in: “Dude, this is not a Medtronic hotline,” he writes. “This is DIY! . . . Brave new world, my friend.”
I imagine everyone laughing. But I’m worried.
Riddell gets serious and suggests that I twist the pump hard to the right—“Like you’re going to break it.”
I follow his unorthodox instructions, twisting and pressing down on the pump’s electronics. For some reason, it works, and the pump is jolted back to life. In my personal narrative, this feels like an initiation—the moment I gain control over diabetes. But deep down, I understand that these things are fickle: the used pump can go down at any moment; the phone, the RileyLink, the CGM—all are vulnerable. Rather than letting it terrify me, though, I accept this new reality. Maybe that’s the underlying story of any chronic illness: how close we all are to breaking.
I’ve now been on Loop for nearly two years. I wake every morning to near-perfect blood sugar. The burden of hours has lessened; life with diabetes has felt easier. And our movement has been expanding. In the months since I started, the Looped Facebook group has grown exponentially, surpassing 15,000 members. Earlier this spring, the Omnipod, another commercial pump, became Loop compatible, bringing in more diabetics who were keen to join this transnational experiment. We’ve been getting notice from other device manufacturers too. Medtronic recently released the MiniMed 670G, technically considered a hybrid closed loop, and the device has been approved by Health Canada. (Though, from what I’ve gathered, many Loopers still prefer the DIY system because it’s more user friendly and customizable.) And, in a gesture that shocked many, Medtronic recently announced that it will work with the FDA and competitor Dexcom to let their insulin pumps and CGMs speak to one another via Bluetooth and an app called Tidepool—essentially Loop gone legit. Original Loop creators, including Pete Schwamb, are involved in the ongoing regulatory discussions, while others, including Ben West, are working on new-product development with various medical companies. It will still take some time for all of this to be approved—in the US as well as in Canada—but it feels like patients are finally leading the way.
Later, I reconnect with Kate Farnsworth. I want to know what’s going to happen when a government-approved artificial pancreas as good as Loop—or better—is finally available. I ask if it will bother her to lose this close community she’s helped create. “Honestly, I would love to be put out of my volunteer job,” she says.
Lately, I’ve been thinking about how I will feel when that day comes. After all, Loop has changed my relationship with my health and with myself—life is more than just a report card, diabetes more than a mere flaw. I’ve become a man verging on cyborg, made up of skin and muscle, tubes and gadgets, all held together by an incomprehensible language. What is this body? I ask myself now. And what could it be?
Correction January 9, 2020: The article stated that, in creating Loop, Nate Racklyeft and Pete Schwamb improved the user interface of work released by other developers. In fact, they created their own insulin dosing algorithm. The Walrus regrets the error.
Correction January 16, 2020: An earlier version of this story stated that Frederick Banting discovered insulin. In fact, he led the team that made the discovery. The Walrus regrets the error.





