In the fall of 1918,the Canadian army began rounding up soldiers at camps in the Maritimes, Quebec, and Ontario. The troops were to join an international coalition to intervene in the Russian Civil War and defend Western liberalism against Bolshevik socialism. Needless to say, the operation failed to reverse the Soviet Revolution, but it succeeded in bringing a second wave of Spanish flu to central and western Canada.
In his groundbreaking 2013 book, The Last Plague, Mark Osborne Humphries charts the cursed journey of the Ocean Limited train, which pulled out of Halifax on September 27, 1918, its cars packed with recruits. The men were to be carried to Victoria, where they would board Siberia-bound ships. Some had been exposed to the flu in Sydney, Nova Scotia, and once the train reached Moncton, several were visibly ill. In Montreal, two of the sickest were carried off to the hospital; in their place, forty-two new soldiers got on.
The Ocean Limited and two similar troop trains continued their journey, picking up men, exposing them to the virus, and depositing the infected in cities across the country—Toronto, Winnipeg, Calgary, Vancouver. Because the mission was secret, local public health authorities weren’t warned of the trains’ arrivals. Soon, cities were inundated: an outbreak in eastern and central Canada had been transformed into a countrywide crisis.
The Ocean Limited episode helps explain why, once the pandemic subsided, Canadians got angry. The war had brought an upswing in patriotism, but as the conflict wound down and reports about the deadly operation circulated, citizens realized the state had not only failed to protect them from the virus but had negligently and cavalierly spread it. They expressed their displeasure through electoral revolts and citywide strikes.
This isn’t surprising. Plagues often bring social turmoil. In fourteenth-century England, the Black Death wiped out between 30 and 60 percent of the population, creating labour shortages among peasants, who used their newfound leverage to win higher wages and the right to own land. Disease outbreaks also magnify inequality, making the poor poorer, the sick sicker, and the angry angrier. In 1832, cholera—an illness that disproportionately affected working class people—ravaged Great Britain and Ireland, fomenting class resentment and ultimately riots in Liverpool, Aberdeen, Glasgow, and Dublin. And, in the 1980s, aids decimated Haiti’s tourist economy, deepening poverty and leading to the uprising that toppled the dictator Jean-Claude Duvalier.
covid-19 has reminded us that plagues shake things up. In Lebanon, where uprisings over corruption and economic mismanagement were underway prior to the outbreak, protests have been reinvigorated, this time with more violence. Merchants in Wuhan, China, have staged sit-ins in anger at having to pay rent for shuttered business properties. Hundreds of migrant workers in Mumbai have stormed a railway station in opposition to lockdown orders that prevented them from returning home. And, in poor suburbs across Paris, residents—angry at the heavy-handed police tactics used to enforce lockdowns—have torched vehicles and lobbed projectiles at cops.
Much as they infect the body, pandemics infect the body politic. They move through our social systems, finding vulnerabilities to exploit. In the process, they lay bare those vulnerabilities to scrutiny—and afford opportunities for self-reflection. The Spanish flu brought a reckoning and, in time, made Canada a better country. covid-19 could do the same.
There are few moments in Canadian history when the federal government was more powerful than it was in 1918. Prime Minister Robert Borden, a Conservative, increased his majority when many opposition Liberals joined him in support of his conscription policy. As the Borden government ballooned in size—hiking taxes, nationalizing rail services, and expropriating power generators—its leaders justified the expansion not only as a necessary war measure but as a means of improving social welfare. Voters expected their government to bring education, health care, and urban sanitation to those who needed it.
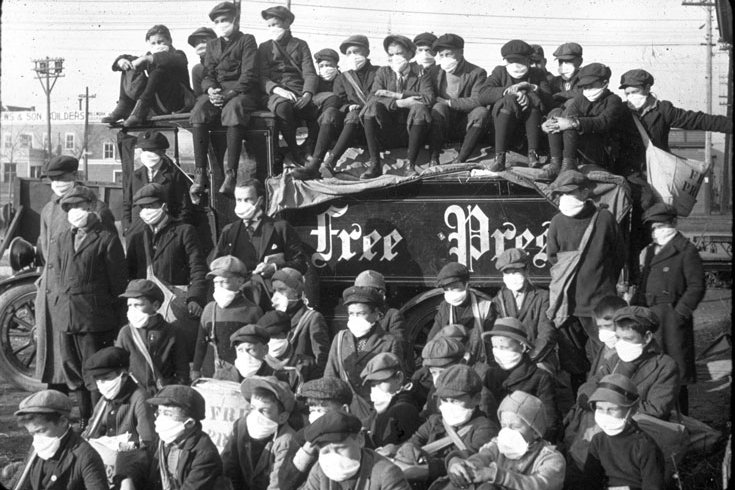
The flu, however, forced them to confront the gap between such lofty aspirations and grim reality. For the most part, citizens had accepted battlefield casualties as the necessary cost of war. But the influenza deaths now happening in overcrowded army barracks and infirmaries were less ennobling. If it was difficult, after the Ocean Limited debacle, for people to view the army as a public-spirited institution—the Edmonton Bulletin decried the “criminal negligence” of military authorities—it became impossible for them to kid themselves about the kind of society their ruling class was building. Public health officials and volunteers were shocked by what they saw in the urban slums: people huddled in sunless, subterranean squalor and, in one case, sick children sleeping in beds where family members had recently died. In poor neighbourhoods, the flu could be twice as deadly as in affluent precincts, and on First Nations reserves, it was five times more lethal than in the country at large.
Such revelations were bound to have political consequences. When Borden resigned, in 1920, he left a party destined for the opposition benches for most of the next four decades. The antimilitary backlash contributed to the resurgence of the pacifist movement, and the flu galvanized Indigenous activists, creating profound doubts about the effectiveness of settler medicine and the benevolence of state institutions. It’s surely no coincidence that the League of Indians of Canada—a forerunner to the contemporary Assembly of First Nations—was founded in September 1919 with a statement that included demands for better health conditions on reserves.
Equally consequential was the spate of workers’ revolts across the country. Esyllt Jones, a labour historian, argues that the pandemic created a sense of aggrieved class solidarity, leading to the famous Winnipeg General Strike of 1919. It isn’t hard to see where such resentment came from. Winnipeg hospitals subjected patients to patronizing questionnaires to assess their ability to pay, a practice that discouraged the poor from showing up at all. Municipal bans on billiards clubs, cinemas, and union halls, enacted in the name of social distancing, seemed pointedly classist, particularly since shops, restaurants, and hotels stayed open. And, because of price gouging among undertakers, grieving workers had to choose between sacrificing months of wages or consigning loved ones to degrading paupers’ funerals provided by the city, which occasionally misplaced the bodies it was supposed to inter. When, in spring, Winnipeggers stormed the streets, derailing trolleys and braving police gunfire—and setting off solidarity strikes from Victoria to Amherst—the humiliations of the pandemic were fresh in their minds.
The 1919 workers’ shutdowns are often credited with politicizing a new generation of labour activists and making social democracy a potent force in Canadian life. Less discussed is the role labour played in reforming public health. Spurred by the pandemic, the newly energized labour press—along with women’s movements and national elites, like writer Stephen Leacock and prime-minister-in-waiting William Lyon Mackenzie King—called for a centralized health bureaucracy that might prevent catastrophes like the Ocean Limited. In 1919, the federal government founded the Department of Health to provide a coordinated response to the next outbreak. But the office kept growing. Soon, it was assisting with food-safety inspections, enforcing sanitation on trains and steamships, operating a network of free clinics, and providing mass vaccinations against diphtheria, smallpox, and scarlet fever. Universal health care wouldn’t arrive until the ’60s, but these earlier developments were important steps in that direction.
In crucial ways, Canada became a better place—more activist, less militarized, with greater political diversity and a larger role for the state in maintaining social welfare. To that end, few national institutions would prove as vital as the new Department of Health (later renamed Health Canada), which went on to combat polio in 1953, h2n2 in 1957, sars in 2003, and h1n1 in 2009—keeping rates of infection and death well below what they would otherwise have been.
Which brings us to the present. Today, federal power isn’t as consolidated as it was during the First World War, the social safety net is more robust, and trust in government remains, for the moment, high. Yet there are uncanny parallels to the crisis of 102 years ago. In some communities, covid-19 is an inconvenience. In others, it’s a source of grotesque suffering—the kind people aren’t supposed to experience in a prosperous democracy.
We’ve learned, for instance, that in long-term-care centres, where more than 80 percent of covid-19 deaths have occurred, people often sleep two or three to a room, and the ratio of patients to workers can be as stark as sixty to one. We’ve learned that Canadian jails, while outfitted with the trappings of modernity—electromechanical locks, digital surveillance cameras—are not designed to achieve anything like modern sanitation standards. (More than half of the inmates at the Joliette Institution, in Quebec, and more than a third at the medium-security wing of the Mission Institution, in British Columbia, have tested positive for the virus.)
We’ve also learned that, in Toronto, the neighbourhoods hardest hit by covid-19 are those where high numbers of Black Canadians reside. We’ve learned that, in some Indigenous communities—like the Dene village of La Loche, Saskatchewan, which has seen more than 150 infections—the risk of illness is exacerbated by housing shortages, overcrowding, and limited access to potable water. And we’ve learned that the urban shelter system—our society’s cut-rate response to the post-1980 surge in homelessness—barely provides adequate shelter at all. Many such facilities resemble the ad hoc havens that spring up after natural disasters: gymnasiums with mattresses spaced seventy-five centimetres apart. (Toronto’s Willowdale Welcome Shelter, which houses refugees, has had over 180 infections.)
The politics of the pandemic have become the politics of everything. Labour organizers bearing megaphones have descended on the Cargill abattoir in High River, Alberta, where nearly 1,000 low-wage workers have fallen sick. At the Saskatchewan Penitentiary, in Prince Albert, prisoners carried out a civil-disobedience campaign in response to lockdowns that confined them to cells twenty hours a day. On April 9, outside the Bradford Valley Care Centre, in southern Ontario, staff members held signs emblazoned with a short plea: “HELP US.” And countrywide protests in solidarity with George Floyd, killed in late May by a police officer in Minneapolis, have drawn attention to the social maladies—poverty, violent policing, unequal access to health resources—that make life dangerous for Black Canadians.
The most contentious social questions will surely work their way through the courts. The Canadian Civil Liberties Association recently filed a lawsuit against the City of Toronto, alleging that conditions in homeless shelters violate citizens’ Charter rights to life and security. So far, nineteen covid-19–related class-action suits have been launched in Canada, and these are only the first drops in what will likely be a torrent of litigation. To read the court documents related to shelters and nursing homes is to get a window into a world of pain, anguish, and rage. The statement of claim in a proposed class-action suit against an Ontario-based long-term-care provider lays out harrowing circumstances: patients who were confined in their rooms for days as their peers died around them, families who found out that loved ones had contracted the virus only when they were issued death certificates.
Over the last few months, Canadians have had the unpleasant experience of looking more closely at their country than they might have wanted to. Plagues have that effect. But, if they reveal uncomfortable truths, they also provide an opportunity to respond. The recent Canadian Emergency Response Benefit in some ways resembles a guaranteed-minimum-income program: it offers no-fuss cash transfers to people in need. In several provinces, the justice system has released inmates through early discharges, passes, and generous bail conditions: such interventions constitute a kind of short-term prison-reform initiative, which could pave the way for permanent changes. And, by making belated efforts to move some shelter residents into single-unit dwellings (often vacant hotels), local governments have accomplished, on a small scale, what housing-first activists have been demanding countrywide: a top-down campaign to give homeless people homes.
As in 1918, a virus is showing not only where the nation is broken but how it might be fixed. The pandemic has “compelled us to see our weakness through tears and sorrow,” reads an op-ed from the Alberta Non-Partisan. “The old way of dealing with the matter of public health can no longer be tolerated.” These lines are from 1918. They could’ve been written today.