EDUCATION
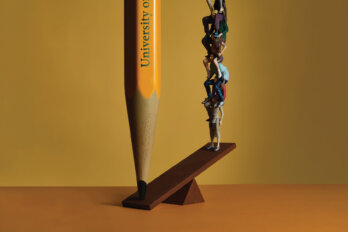
Inside the Mental Health Crisis Facing College and University Students
Campuses are offering more wellness programming than ever before, so why are rates of student mental illness on the rise?
BY SIMON LEWSEN
PHOTOGRAPHY BY CHLOË ELLINGSON
Published 02:39pm, Oct. 26, 2021
Listen to an audio version of this story
For more audio from The Walrus, subscribe to AMI-audio podcasts on iTunes.
In the summer of 2012, Sope Owoaje, then fifteen, travelled from Brampton, Ontario, to her hometown of Lagos, Nigeria, to attend her cousin’s wedding. In Yoruba culture, weddings are extravagant affairs. Owoaje recalls that her father, a Lagos resident and executive at the central bank, paid for the entire event and walked the bride down the aisle.
Following a church ceremony on the third day of the festivities, Owoaje and her cousins returned to the family home for one last celebratory dinner. Her dad’s car arrived a minute later, trailed by four strange men on motorcycles. Suddenly, a motorcyclist darted in front of the vehicle, cutting it off, while the other three crowded in. Owoaje watched as one of the men pulled out a gun and shot her father through the window of the car. “The bullet missed his chest and hit his upper arm,” Owoaje says. “Everybody around me screamed. My dad had a rush of adrenaline. I saw him speed past me with his window shattered.”
He drove himself to an emergency ward, where doctors hurried him into surgery. Despite the injury, he recovered fully, and the family chalked up the violence to an attempted carjacking. But, when Owoaje returned to Brampton, she felt changed. She withdrew from social life and her grades slipped. She replayed the shooting in her head and felt unsafe everywhere she went. “I was scared to be in rooms where I couldn’t see the entrance,” she says. “I needed to keep track of how many people were present, who was coming and going, and where the doors were located.”


When she was in grade twelve, her mother took a new job and moved the family to Iqaluit. The wide streetscapes of her new hometown gave Owoaje a sense of restfulness, and Inuit culture, with its storytelling traditions and reverence for Elders, reminded her of her Yoruba upbringing. She often visited the Elders’ Qammaq, a community centre where seniors gathered to talk. An Inuk woman in her nineties told Owoaje about how the residential school system had broken her family, and other people described being taken by ship to tuberculosis asylums where their friends died and were buried in unmarked graves. Owoaje began to understand trauma—how it stays with you and manifests in unpredictable ways.
In Iqaluit, she began to heal, but when, in the fall of 2014, she moved to Winnipeg to study life sciences at the University of Manitoba, her anxiety returned. During orientation week, she had a fever that consigned her to her thirteenth-floor dorm room. When she emerged, it appeared that everybody except her had made new friends. “I was more lonely than I’d ever been in my life,” she says. For lectures, she’d show up early to pick an optimal seat—sufficiently close to the exits to enable a speedy escape but far enough away that she wouldn’t be in the line of fire if a shooter came in. “If I got to class and saw that somebody had taken my spot,” Owoaje says, “I would go back to my dorm room furious with myself.” She had expected university to be exhilarating, but instead, she felt terrified and unexcited to learn.
She wanted professional help but couldn’t find an online link to student mental health services. She called the campus medical clinic instead and, after three weeks, received an appointment. “I told the doctor, ‘I need mental health counselling,’” Owoaje recalls. “And he said, ‘Sorry, we only deal with physical issues here.’” Clearly, she’d gone to the wrong place, but he didn’t mention where the right place might be. (In an email to The Walrus, a spokesperson for the University of Manitoba wrote that the school offers “an integrated continuum of care, and a ‘no wrong door’ philosophy to ensure students are directed to the services they need.” The spokesperson did not comment on the specifics of Owoaje’s experience.)
Owoaje felt rebuffed, as if the university were chastising her for failing to keep herself together. What she didn’t tell the physician was that even getting to the clinic had been an ordeal. “It was at the end of a long, dark corridor,” she remembers. “I knew that, if I went far enough down that hallway, I wouldn’t be able to see the exits.”
Although owoaje’s story is extreme, her frustrating experiences with the university health bureaucracy are common. Over the last decade, reports of postsecondary students trying and failing to secure psychological services have become ubiquitous. Pundits and psychiatrists now talk about a mental health crisis on campus, and it isn’t hard to see why.
In 2019, the National College Health Assessment, which surveys students at Canadian postsecondary institutions, found that almost 70 percent said they had felt “overwhelming anxiety” in the previous twelve months, and more than half said they were living with debilitating depression.
The same study found that over 16 percent of students had seriously considered suicide, an increase from 10 percent in 2013. Reported suicides on campus are a fraction of the overall numbers, but even these figures are shocking: six at the University of Ottawa during the year leading up to April 2020 and another suspected five at the University of Alberta during the two years before that. Since 2018, a single building at the University of Toronto—the Bahen Centre for Information Technology—has had three student deaths in its atrium alone.
Universities have responded by expanding their mental health resources, running resilience workshops, and hosting meditation sessions. But Owoaje’s experiences—and those of numerous other young people—suggest that many institutions still misunderstand the crisis, which has little to do with a lack of wellness programming or mindfulness training and a great deal to do with shifting demographics and the changing role of the university in our society.
When we imagine the typical student who seeks psychological services on campus, we might picture a young adult who is struggling to handle the stress of assignment deadlines and exams. We don’t picture somebody like Owoaje, who continues to suffer side effects from a traumatic event she lived through. But people arrive on campuses today with a wide—and ever-widening—range of life experiences.
In 2001, 14 percent of postsecondary students in Canada identified as visible minorities; by 2019, that figure was 44 percent. Over roughly the same period, the number of new international students in the country jumped from 70,000 to 250,000. Statistics Canada does not collect class-based data on postsecondary enrolment, but one 2010 survey shows that half of students—compared with one-quarter in the mid ’70s—worked part-time jobs while studying.
Clearly, a student seeking mental health support today can be affluent or poor, Canadian or foreign born. And, while some are struggling with the circumstantial stresses of university life—independent living, time management, friend-group formation, and academic pressure—others are contending with highly individualized experiences. Psychologists have long known that the results of such traumas often manifest between the ages of eighteen and twenty-five, just as students in our crowded postsecondary system embark on what has become a financially precarious, emotionally exhausting phase in their lives.
Critically, the campus mental health crisis predates COVID-19. Of course, nobody would argue that the pandemic has been good for psychiatric health. As universities have transitioned to remote learning, students have found themselves isolated from friends, health care providers, and support networks—the latter being particularly important among queer and trans youth, who may depend on one another for self-affirmation. It’s tempting to assume that, as campus life normalizes, the crisis will return to the prepandemic status quo, but the status quo was dire to begin with. When it comes to student mental health, the worst that can be said of COVID-19 is that it exacerbated a problem it didn’t create.
“I learned that, if you go to the health and wellness centre and say, ‘I’m dealing with depression and anxiety,’ they’ll respond, ‘You’re not in critical need of support,’” Sarah says. “But, the moment you say, ‘I have a plan to kill myself,’ they’ll throw you in handcuffs.”
Ashley has been a perfectionist for as long as she can remember, a tendency she attributes, in part, to her relationship with her father. She recalls that he belittled her constantly. “He’d tell me I was stupid and worthless and destined to die alone,” she says. “I thought, ‘If my own father is saying these things, they must be true.’” To prove him wrong and to establish a sense of control, she threw herself into her studies, seeking not just excellence but flawlessness. If she got 95 percent on a test, she’d soon be crying in the washroom. (To protect her identity, Ashley’s last name has been withheld.)
Her parents separated when she was young, and she was shunted between two homes. At thirteen, she returned from a trip abroad and abruptly announced that she was cutting ties with her father. She didn’t want to live with him or see him for weekly visits, and it soon became clear that he would no longer fund her future university education, a realization that increased her academic anxiety. Like many Canadians aiming to get a degree, Ashley now faced the prospect of taking on years of debt. “I told myself I needed to work my ass off to get a scholarship,” she says.
In 2018, she arrived at St. Thomas University, in Fredericton, to study criminology and psychology. She had received a full scholarship—a clear victory, although it didn’t feel like one. To keep her funding, she needed a 3.7 GPA, and to get into law school, she needed to do even better. Reasoning that a strong resumé couldn’t hurt, she packed her schedule with courses, extracurriculars, and part-time retail jobs. Her days felt joyless and exhausting. The insomnia and nightmares she’d experienced as a teenager returned, as did chest pains, loss of appetite, and recurring crises of confidence.


She’d been warned that university grades tend to be lower than high school grades, but she wasn’t prepared for her first A-minus, on a 300-level criminology course she’d taken in first year. Was it good enough, she wondered, to warrant a partially or fully funded law school placement? She’d always been one of the highest achievers she knew. If she was no longer that, what was she? Had her high school successes been a mirage? Had her father been right about her all along?
A great deal has been written about why students today experience extreme self-doubt and anxiety, but many of these theories neglect to reckon with trauma or familial and financial pressures. The crisis is sometimes attributed to social media. Online discourse, after all, can be toxic and polarizing, image-based platforms like Instagram wreak havoc on self-esteem, and tech-mediated connections are a dismal replacement for in-person relationships. Another explanation focuses on a growing child-rearing trend among middle- to upper-class families—sometimes called intensive or helicopter parenting—in which parents subject their children to constant supervision and extracurricular activities, depriving them of opportunities to build resilience and emotional independence.
Both hypotheses offer convincing if not fully satisfactory explanations. The social media theory attributes problems at Canadian schools to tech companies in faraway Palo Alto and Beijing, and the intensive-parenting theory fails to account for students, like Owoaje and Ashley, who weren’t raised in the kinds of hypercompetitive households where such parenting practices are prevalent.
To fully understand the present crisis, one has to appreciate a fundamental and often overlooked fact: higher education is not what it used to be. Not only do we have a more diverse student body with equally diverse psychiatric needs, we also have an academic culture that has changed profoundly in the past six decades, making the university experience more stressful than it once was. The classic liberal conception of postsecondary institutions as places where young people take a kind of sabbatical from life—read the great books, engage in endless debates, and learn to see themselves as citizens—has given way to a new model, more narrowly vocational in focus.
If you attended a Canadian university in, say, 1961, you were probably white, Canadian born, and part of a small, economically secure demographic. (That year, there were only 130,000 full-time students in the country. Today, the number is nine times that.) What’s more, you were probably pursuing your studies out of intrinsic rather than vocational motivations. “It was easier back then to have a middle-class lifestyle without a university degree,” says Alex Usher, president of the consulting firm Higher Education Strategy Associates.
In the decades that followed, things slowly shifted. First came the economic downturn of the 1970s, which brought a new era of class stratification. The prosperity gap between an increasingly credentialized professional elite and a less-educated economic underclass began to widen and hasn’t stopped since. Then came the early ’90s recession, which saw both dramatic cuts in government funding to higher education and two-fold increases in tuition. By this point, universities had become both less affordable and more necessary than before. “The cost of education went up,” says Usher, “but people became more—not less—likely to enrol, because white-collar labour was now valued so much more relative to unskilled labour.”
In the twenty-first century, skyrocketing property values further increased students’ cost of living in some parts of the country. By 2018, average student debt at graduation had more than tripled since the early ’80s. Schools also got bigger as millennials came of age and universities began aggressively courting international students, who pay vastly more in tuition than their Canadian peers. Between 2000 and 2019, total enrolment at Canadian universities increased by 78 percent, placing new demands on student support systems. Today, the combined population of just three schools—the University of Toronto, York University, and the University of British Columbia—exceeds the number of people enrolled in the entire Canadian system six decades ago.
As campus populations grow, students have reported depersonalized classrooms, making university culture more alienating than before. The National College Health Assessment survey notes that, in 2019, 70 percent of Canadian students experienced extreme loneliness. Rising enrolment numbers have also contributed to a sense among young people—perhaps more illusory than real but strongly felt nevertheless—that they are jockeying in a crowded arena for a dwindling number of jobs. By historical standards, the employment market for university graduates in Canada is far from terrible, but students nevertheless fear joblessness. “When young people become extremely anxious, their ability to evaluate future probabilities becomes skewed,” says Steve Mathias, a psychiatrist and the executive director of Foundry, a network of youth mental health clinics in British Columbia. “Students will say things like, ‘If I fail this test, I’ll become homeless and destitute.’”
Our large, multicultural campuses require an equally diverse approach to mental health, with bespoke services tailored to individual student needs. “The point of psychotherapy is meeting the clients where they are.”
These combined stressors put immense pressure on young people to prioritize scholastic pursuits over other opportunities—for aimless reading, say, or romantic and sexual exploration—that campus culture can offer. Like their American counterparts, Canadian students now compete fiercely for prestigious undergraduate placements—software engineering at the University of Waterloo, commerce at the University of British Columbia, health sciences at McMaster University—and then more fiercely still for a limited number of postgraduate slots, many of which require A-level transcripts. “We have an education system that starts talking about university in elementary school,” says Joanna Henderson, director of the Margaret and Wallace McCain Centre for Child, Youth, and Family Mental Health, in Toronto. “Students are expected to build their postsecondary applications by taking leadership roles, getting top grades, and excelling at STEM. They work tremendously hard to arrive at this destination only to realize that it’s not an end point but a beginning.”
By prioritizing high achievers, Henderson argues, universities are selecting not only for diligent candidates but also for those who view scholastic success as central to their identities. For such students, a bad grade can be destabilizing. When that grade appears on an exam worth 80 percent of a final course mark, or when it comes from a harried teaching assistant who doesn’t offer in-depth feedback, students can feel like they are losing a game whose rules were never explained. Imagine being told all your life that you are ahead of the pack and that you must stay there, both to secure a stable future and to get a return on the investments that family members or granting agencies have made on your behalf. Then, imagine falling behind, for reasons you don’t understand, at the precise moment when staying on top feels more critical than ever before. Furthermore, imagine that you are contending with profound loneliness, past trauma, and financial insecurity, all while working a part-time job with the usual mix of erratic hours.
Such stressors can lead to sleep disruption, irregular eating, and substance abuse—all of which correlate with mental illness—or they can trigger preexisting psychiatric conditions. They can deplete reserves of neurochemicals, like dopamine and serotonin, needed to sustain a sense of well-being, or they can flood the brain and body with cortisol, the stress hormone, which, in excess, can push people into near-constant states of anxiety, making it difficult to conceptualize daily challenges in a proportionate or healthy way. They can also lead to identity confusion and an acute sense of shame. “When you think about predictors of suicide, an important in-the-moment factor is relationship disruption,” says Henderson. In her clinical practice, she often sees young people who are upset about their university grades—and who, when expressing these feelings, immediately mention their families. “They say things like ‘My parents are going to be so disappointed in me’ or ‘My parents are going to kill me.’”
Of course, university has always been challenging, but Juveria Zaheer, a clinician scientist and medical head of the emergency department at the Centre for Addiction and Mental Health (CAMH), in Toronto, says that the stakes seem higher today than ever before. For many students, an undergraduate degree can feel like a four-year, $30,000 gamble. “There’s a reason adults have dreams that they’ve missed an exam,” says Zaheer. “It’s a primal fear. Young people are actually living those nightmares.”


During her shifts at the emergency department, Zaheer frequently sees youth patients in severe psychiatric distress. “When they get to us, a lot of difficult things have already happened in their lives,” she says. “They come not with one problem but with several—intense suicidal thoughts, panic attacks, deteriorating social relationships. Often, I’m the first psychiatrist they’ve seen. It’s worrisome that so many young people are making their initial presentation for mental health care at an emergency department.”
It’s hardly surprising, though. Just as postsecondary institutions have misunderstood the causes of this crisis, they have miscalculated the solutions. In Canada, Zaheer argues, upstream funding for mental health supports on campus could help prevent serious mental health presentations at acute care downstream. Canadian mental health care is funded primarily by federal contributions to provincial health budgets. But the system is two tiered: anybody with a health card can see a doctor who’s licensed to prescribe psychotropic medications, but psychological services, like cognitive behavioural therapy or interpersonal psychotherapy, are mostly covered by workplace insurance plans or must be paid for out of pocket. (There are exceptions to this rule. The system sometimes offers free counselling to people who’ve been hospitalized for mental illness, and nonprofit clinics across the country, many with limited means, also deliver affordable therapeutic services to patients in need.)
Like the Canadian system writ large, campuses provide too little by way of sustained, patient-focused support. At many schools, sessions with mental health counsellors go either to students in acute distress or to those who’ve waited their turn in the queue. In extreme cases, students may wait up to two months for basic counselling. Outreach is a problem too. A 2020 survey of six Canadian universities showed that only 56 percent of students were even aware of the mental health services their campuses offered.
Moreover, the services themselves aren’t as flexible as they could be. Most involve a fifty-minute meeting (or a limited number of such meetings) booked in advance. “Some people can do remarkably well with short-term interventions,” says Amy Gajaria, a child and adolescent psychiatrist at CAMH. “But there are other people—those who’ve been dealing with mental health challenges since childhood or those with trauma and comorbid substance-abuse problems—for whom even two or three months of counselling isn’t enough.”
When treating young adults, clinicians need time just to arrive at a diagnosis. If an eighteen-year-old first-year student suddenly starts drinking heavily and burning through scholarship money, is she having a manic episode or behaving like a teenager who’s finally away from home? “A lot of illnesses present in young-adult populations,” Gajaria says. “But there’s also diagnostic uncertainty because the brain is still evolving. It’s best to get to know a patient over several months, but our system isn’t set up for us to do that.”
She adds that, on campus, specific types of services are woefully undersupplied, like dialectical behavioural therapy, which can treat borderline personality disorder, or trauma therapy, which is complex and time intensive. There’s also a lack of culturally relevant services: counselling in languages other than English, therapies that are integrated into spiritual practices, or Indigenous programs that involve spending time on the land. Of course, universities and colleges can always refer students to off-campus resources, but these, too, are overstretched and underfunded, and private care can easily cost $200 per session. “The wait for publicly available trauma therapy can take up to two years,” says Gajaria. “Should we really be asking an eighteen-year-old in distress to wait that long for treatment?”
Mathias, the Foundry executive director, argues that what’s missing from campus services—and from the Canadian system more generally—is a sense of balance. “Our system provides a narrow scope of interventions to young people who have lost a great deal of their function to mental illness,” he says. “But we don’t assign resources to those who are just starting to struggle or who are struggling just a bit. Young people are falling off a cliff. We’re putting doctors and hospitals at the base to catch them, but we’re failing to prevent the fall itself.”


This is what happened to Sarah, a life sciences student at the University of Toronto. (To protect her identity, Sarah’s real name has been withheld.) When she stepped into the exam room for her first midterm test, in organic chemistry, she felt nervous but ready. She’d studied diligently, attended every class, and uploaded her lecture notes to the course website for the benefit of fellow students. But the ambience of the room was stifling. “I have a fear of crowds,” she says. “I could hear people shuffling around me, and I could feel their stress.” The proctor set the test in front of her, and her mind went blank. “I looked at the page and thought, ‘I don’t know any of this. It’s like a foreign language.’”
A week later, the professor returned the test and posted anonymized grade data on the overhead projector, revealing that Sarah had scored 35 percent, one of the lowest marks in the class. She ran from the lecture hall crying. As an international student from the Middle East, Sarah feared that, if she failed too many courses, her visa might be revoked. The exam incident soon metastasized into a general sense of disquiet—a similar, if heightened, version of the anxiety she’d experienced for much of her teenage life.
At an appointment with the school’s health and wellness centre a few weeks later, she explained to a campus doctor that her mental health was spiralling. “I asked, ‘Can I see a counsellor?’” she recalls. “He said, ‘Not really. There’s a wait list, and it’s for people who need more help than you do.’” He suggested she might have ADHD and gave her a prescription for clonazepam—a tranquilizer in the benzodiazepine family—for which a known side effect is depression. “Suddenly, I was crying every day,” Sarah says.
In her second semester, she switched to mirtazapine, an anxiety medication, at which point she developed irritable bowel syndrome. At the time, she assumed the IBS was caused by the medication, though she now suspects that the link might be coincidental. Nevertheless, the condition was so severe that she could rarely sit through a full tutorial or quiz. “It was horrible,” she says. “I’d gone from anxiety to depression to IBS in a single year. I was like, ‘What’s going to happen next?’” She did manage, however, to register with accessibility services and receive additional time to complete her exams, at which point her grades improved.
In her second year, she moved out of residence and into an apartment in Toronto’s Kensington Market neighbourhood. To make rent, she took a night job at the university, a position that required her to walk to campus at 11:30 p.m. On the way, she was often followed, cat-called, or verbally harassed. “A lady yelled, ‘I’m going to fucking shoot you in the head and rape you, bitch,’” Sarah recalls. “I’d never experienced that kind of language before. I felt like it was my fault, like I was doing something to bring out that anger in people.” Her IBS made social life difficult. “Other people could go out and eat together,” she says, “but I couldn’t get through a meal.” Her exhaustion compounded her loneliness, anxiety, and shame, until she found herself back at the health centre, telling a doctor—a psychiatrist this time—that she no longer wanted to live.
When Sarah had first presented at the clinic, a year earlier, she’d been surprised by the lack of urgency the staff had shown. This time, however, the psychiatrist sprang into action. She got up, called campus police, and told Sarah she was committing her to the in-patient ward at CAMH. “I asked, ‘Is it okay for me to go there myself?’” she says. “And the psychiatrist said no.” When the police arrived, she says, they put her in handcuffs and walked her to the back of a cruiser. It was among the most degrading experiences of her life.
In an email to The Walrus, Sandy Welsh, vice-provost of students at the University of Toronto, said that such incidents, involving police and handcuffs, are uncommon. “In situations where a student requires urgent care from specialized mental health support services, University staff will work with the student to arrange voluntary transportation to hospital, whenever possible,” she wrote. “Campus police may be called upon to assist with transporting a student to hospital when all other options have been exhausted.” She added that the university is currently reviewing its policies and procedures for handling such emergencies.
Nevertheless, at the University of Toronto, this incident—and others like it—quickly became campus lore. Students warned one another about the risks of seeking mental health services. Sarah was outraged not only for having been treated like a criminal but also for having been denied earlier therapies that might have made such extreme interventions unnecessary. “I learned that, if you go to health and wellness and say, ‘I’m dealing with depression and anxiety,’ they’ll respond, ‘You’re not in critical need of support,’” she says. “But, the moment you say, ‘I have a plan to kill myself,’ they’ll throw you in handcuffs.”
Universities and colleges were never intended to be psychiatric institutions, and administrators are perhaps justified in wondering whether the mental health crisis is theirs to solve. But the fact remains that the undergraduate years are an incredibly tumultuous period in a person’s life. “About 70 percent of mental disorders first arise in adolescence and young adulthood,” says Emily Jenkins, a professor at the University of British Columbia’s school of nursing who specializes in substance use. “This phase coincides with students’ arrival on campus and often their departure from home, which, in itself, can be destabilizing.” Surely, Jenkins argues, this implies some obligation on the part of the academy toward the young people in its care.
Of course, universities can’t tackle the problem alone. Gajaria, the CAMH child-and-adolescent psychiatrist, argues that Canada urgently needs a sustained federal and provincial investment in psychiatric care. (Ahead of the fall federal election, the Liberals, the Conservatives, and the NDP committed to increasing funding for mental health care. The Liberal Party also said it would support the hiring of up to 1,200 counsellors at universities and colleges.)
Postsecondary institutions will never be able to provide the full suite of mental health services, but they should be able to give swift referrals to clinicians and counsellors in the public sector. “The worst part of my job,” says Gajaria, “is knowing what my patients need but being unable to get it for them.” Parents, too, can help mitigate the crisis by talking to their university-age children about mental health and by reminding them that low grades and academic adversity aren’t signs of personal failure but, with the right support, could be opportunities for emotional growth.
Universities are increasingly investing in a range of early intervention therapeutic services with the goal of eliminating wait lists and reducing the number of extreme crises. (To their credit, several schools, including McGill University, the University of British Columbia, the University of Victoria, and the University of Regina, have made major strides in that direction.) In the past decade, campuses have begun facilitating open discussions about mental health, but such dialogues often focus on the safest subject matter: stress, burnout, and self-care. When a school provides leather-crafting workshops and therapy dogs to help students manage anxiety—as the University of Toronto does—but then forcibly sends other students to hospital in police cars and handcuffs, it sends a message: some types of mental illness will be supported here while others will be treated like crimes. “As soon as campus administrators hear words or phrases like suicide or psychosis or eating disorder, they lapse into risk-management mode,” says Henderson, the McCain Centre director. “They say, ‘Oh my God, I’d better take action or something bad is going to happen.’ They need to recognize that turning a young person away from early intervention services is also a risk. Calling the police is a risk. You can end up traumatizing the student.”
Beyond that, schools might innovate. Different universities could experiment with different approaches, all the while collecting data on what works and what doesn’t. In time, these experiments may yield a set of best practices to be deployed nationally. Perhaps they will include initiatives at the University of British Columbia and McGill University to create a centralized hub—a single office, like a port of entry—where students get an adviser who sets up appointments for them and helps them navigate the campus health bureaucracy. Or perhaps such best practices will include the University of Ottawa’s initiative to train teaching and administrative staff in basic mental health care. The goal isn’t to turn professors into therapists; rather, it is to show them how best to communicate with students in distress and to give them an up-to-date list of campus resources.
Among the most successful programs are those that recognize the diversity within student bodies and zero in on specific communities. In 2005, the University of British Columbia opened a satellite campus in the Okanagan Valley, on unceded Syilx Okanagan territory. Two years later, it pledged to admit all Indigenous applicants. Those who didn’t have the grades or high school education to warrant a direct admission could instead join the Access Studies initiative, a year-long program that combines university-level courses with “upgrading courses” in English or math, intensive one-on-one tutoring, weekly workshops on well-being, and Indigenous cultural activities. All Access Studies students are assigned an academic adviser who coaches them as they progress through the program. At the end, they’re eligible to either continue at the University of British Columbia or transfer to any other university in the province.
Ian Cull—a former associate vice-president of students at the Okanagan campus, a member of Dokis First Nation, and an architect of the Access Studies program—sees such initiatives as an alternative to the approach that many universities adopt. It is unreasonable, he argues, to expect all students, even those who’ve faced tremendous adversity, to arrive on campus and demonstrate instant mastery over the academic, social, time-management, and health challenges that await them.
Has the Access Studies program been good for mental health? Cull argues that the completion rates speak for themselves. In the 2020/21 school year, the retention rate for Indigenous students at the Okanagan campus was 84 percent, compared with 89 percent for domestic students at large, and the gap is narrowing. “Our Access students progress through their degrees at roughly the same rate as non-Indigenous students,” he says. “Even the most underprepared Access students are performing as well, by second year, as those who come here through our normal admissions procedures.” Similar programs can be found elsewhere in Canada. The University of Manitoba has its own year-long Access Studies program targeted at Indigenous, racialized, and rural students, as well as those who are newcomers or face economic barriers. The University of Toronto also has a new initiative that aims to recruit prospective Black and multiracial medical students via summer internships and a specialized admissions process.
Like Cull, Omar Patel, a Muslim chaplain, believes he’s found a way to meet the needs of students who are underserved by mainstream campus culture. In 2012, he returned to Canada after completing his divinity training in the UK and South Africa. “I was looking for ways to bring spirituality to the public, particularly young people,” he says. “In the time of the Prophet Muhammad, mosques were places of counselling and therapy. People would come to the Prophet to discuss marital and social concerns. But the mosques of today are primarily focused on prayer. They’ve lost their connections to the original prophetic mosque.”


To help bridge that gap, Patel did a master’s degree in pastoral care at the University of Toronto and took courses at the Toronto Centre for Psychotherapy and Counselling Education, eventually becoming a registered psychotherapist. In 2015, he began working at the university’s Muslim Chaplaincy, where he led Friday prayer services, offered regular counselling sessions, and acted as a liaison between campus administrators and students.
Patel argues that Muslim students reticent to visit the health and wellness centre may be more trusting of religious leaders like him, who are uniquely positioned to address culturally specific conundrums. What, for instance, might a Western-trained, non-Muslim psychotherapist say to a Muslim student who wants to sever relations with an abusive parent while at the same time honouring the Prophet Muhammad’s exhortation to love and forgive one’s kin? Or what might such a psychotherapist say to a student who, because of obsessive-compulsive disorder, is spending half an hour on ablutions for prayer, a process that should take two minutes?
“If a student from a religious Muslim background sees a counsellor who has no connection to the faith,” says Patel, “the student must devote a huge chunk of time to explaining their background. So the problem the student came in with, which should be the focus of the session, doesn’t get proper attention.” Patel acknowledges that Western psychiatry works well for many students, but he argues that, in today’s universities, no single model is sufficient. His opinions are backed by data: a 2009 metastudy from the journal Psychiatric Services shows that, when it comes to psychiatric care, culturally competent approaches reduce disparities in treatment outcomes between minority and majority populations. Initiatives such as Cull’s and Patel’s may be happening on the margins of the mainstream campus health bureaucracy, but administrators would do well to pay attention to them. Our large, multicultural campuses require an equally diverse approach to mental health, with bespoke services tailored to individual student needs. “The point of psychotherapy,” says Patel, “is meeting the clients where they are.”
Sarah left CAMH three days after being committed, only to find herself back at the health and wellness centre, back in handcuffs, and back at the hospital, this time for a month. After her second discharge and a suicide attempt, she registered in an outpatient program at CAMH and finally got access to the thing she’d wanted all along: regular appointments with a cognitive behavioural therapist. “I learned that your thoughts affect your emotions and your emotions affect your thoughts,” she says. “I learned a new vocabulary to label my emotions and to tell people what I’m going through.” By articulating her feelings, she could distance herself from them. The suicidal thoughts, panic attacks, and IBS abated.
During Ashley’s first semester at St. Thomas University, a counsellor on campus asked her a question nobody had put to her before: Was she suffering from PTSD because of her father? Ashley was skeptical (Isn’t PTSD for soldiers?), so she read studies on the condition and asked friends for input. In time, she came to accept the diagnosis. Knowing the cause of her anxiety enabled her to better manage it. Today, she has a mental list of warning signs—joylessness, loss of appetite, loss of interest in physical activity—that alert her when she’s overworked and on the edge of burnout. She will always be a high achiever, she reckons, but success doesn’t have to come at the expense of happiness.
Owoaje eventually decided not to finish her program at the University of Manitoba. She returned to Iqaluit, where she enrolled in the nursing program at Nunavut Arctic College. It was then that she reconnected with Hunter, a high school acquaintance who had been friends with her brother. On their first date, Owoaje and Hunter saw Black Panther at the Astro, the only cinema in town. Hunter had visited the theatre earlier that afternoon to pick a seat where Owoaje would feel safe. Although she’d barely known him before, she felt that she was reuniting with an old friend. She told him the reasons for her PTSD, and he helped her reconnect with her community. “We’d drive around town,” says Owoaje, “and talk about everything we’d missed in each other’s lives.” (To protect his identity, Hunter’s real name has been withheld.)
Hunter was usually cheerful, with an infectious, dimpled smile, but he carried within himself a profound kind of pain. When his mood darkened, he’d turn silent. On bad nights, Owoaje would hold him wordlessly for hours until the storm passed. On good nights, he’d tell her about the activities that helped him reestablish a sense of well-being: hockey, basketball, and hunting, an Inuit tradition he found therapeutic. “Seals have delicate hearing. They pick up on every footfall. So you have to be quiet for hours,” says Owoaje. “You learn patience and humility, and you practise being alone with your thoughts.” With Hunter, Owoaje found what she’d been missing at the University of Manitoba—a sense of connectedness with another person.
Two years after her return to Iqaluit, Owoaje took a solo trip to Paris, London, and Rome. For the first time since they started dating, she and Hunter would spend weeks apart. Hunter’s community, meanwhile, had been selected to go on a narwhal hunt, a rare opportunity. (To preserve the species, the government of Nunavut regulates the number of narwhals that can be culled each year.) He was exhilarated at the prospect of catching a narwhal, an achievement that would surpass anything he’d done as a hunter. He and Owoaje sometimes spoke of the hunt as a healing practice because it allowed him to make plans and look forward to the future. “I said to Hunter, ‘Promise me that you’ll be fine and that you’ll be here when I come back,’” she recalls.
She knew that Hunter’s mental anguish could flare up unexpectedly, but she does not know the specific factors that led him to take his own life while she was abroad. She got the news of Hunter’s death via social media, and on the plane back to Iqaluit, she was inconsolable.
Since then, Owoaje has thrown herself into activism. She started a Nunavut chapter of Jack.org, a national organization dedicated to youth mental wellness. In June 2020, she helped organize a protest outside the Nunavut legislature, calling on the government to increase funding to front line support and establish a mental health facility in the territory. She also ran a massive survey at Inuksuk High School about student mental health needs. The most common need: regular access to a trained counsellor.
Because of her work, she often finds herself reflecting on the duty of care that exists—or should exist—between students and the educational institutions entrusted with their well-being. Had she received the support she required at the University of Manitoba, she wonders, would her experiences there have been salvaged? Had she been less lonely, would her trauma have been easier to manage? She hopes future students will no longer have cause to ask such questions.
Once in a while, she visits her favourite spot, on a hilltop near the school, where she and Hunter used to watch the snowmobiles on the land or the fishers in their boats. If they saw one of his friends heading out on a hunt, they’d often spin a yarn about him getting trapped in a snowbank or firing his gun in the air to scare off a polar bear. Owoaje imagines that Hunter is still with her. He might point out a boat on the water. “I bet they’re going to catch enough Arctic char for the entire community,” he says. “Yes,” she adds, “or maybe they’ll catch a narwhal.”
This article was written and photographed with the financial support of the OCUFA Fellowship in Higher Education Journalism.