The sprawling Medicago facility in suburban Quebec City smells like a botanical garden and sounds like an airplane hangar. Thousands of Nicotiana benthamiana plants, a close cousin of tobacco, grow in long rows amid noisy ventilation. When the plants are six or seven weeks old, maybe twenty centimetres tall, they go on a journey, lined up by the dozens onto a flatbed that’s then inverted over a tank filled with fluid. The plants get dunked. The tank seals. And the roots are trapped in the air between the liquid and the lid, so a vacuum hose can slip into that space and begin to suck.
Listen to an audio version of this story
For more audio from The Walrus, subscribe to AMI-audio podcasts on iTunes.
The plants act like sponges: apply pressure to the roots and the leaves collapse; release that pressure a minute later and they expand, absorbing the liquid deep into their cells. This particular bath is filled with a bacteria that’s been slightly tweaked. Bits of its DNA have been swapped out for DNA from the spike protein of SARS-COV-2, the virus that causes COVID-19.
Once the plants come out of the tank, they’re moved to an incubation chamber, the temperature, light, and humidity tightly controlled. For the next week or so, the bacteria will insert its genetic information into the plants, triggering the production of millions of spike proteins in every cell of the infected leaves. The spikes self-assemble into something called a virus-like particle—not the virus itself but a particle roughly the size and shape of SARS-CoV-2. Gowned workers come and harvest the plants, stripping the leaves like they’re plucking basil for pesto, then send them on a conveyor belt that passes through what’s basically a paper shredder.
The chopped-up leaves head next into a vat of enzymes and are left to soak overnight. The enzymes work to break apart the cell walls, releasing the viruslike particles so they can be collected, purified, and converted into a yellowish vaccine. This doppelgänger for SARS-CoV-2 can’t inflict any real damage, but “when you inject it into someone, the immune system sees it as though it’s the real virus and thinks, Oh my God, there’s an invader here,” says Medicago executive Nathalie Landry. “And then it will trigger a good immune response.”
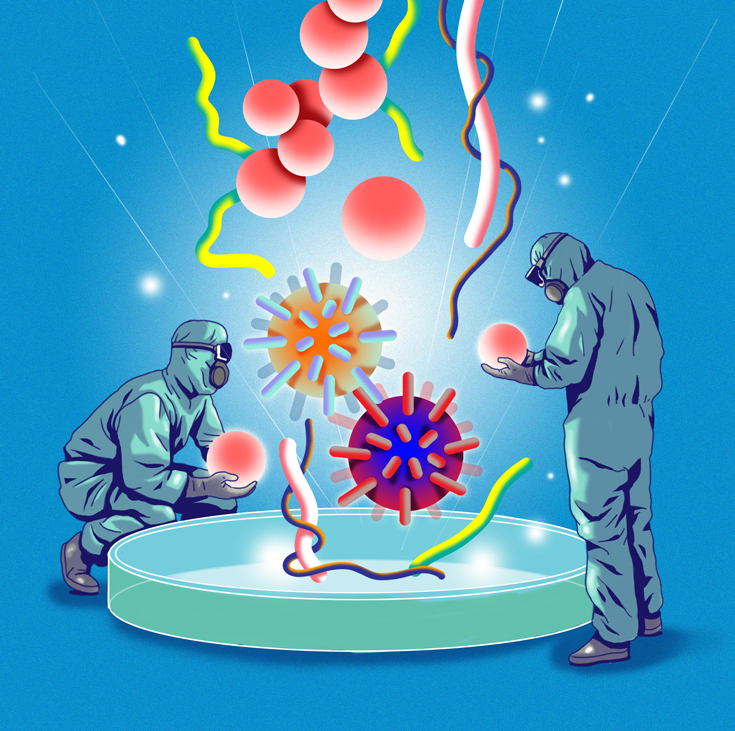
A vaccine is, in essence, a trick—a sleight of hand that convinces your body to mount a counterattack to a given pathogen before that pathogen actually infects you. There are various ways to pull the trick off: vaccines can be made with a weakened virus, or a killed virus, or just a key part of the virus, or a part of the virus piggybacking on a different, benign virus, or an instruction manual for making that part of the virus yourself. In each approach, you get the benefits of an immune response without the messy business of a disease.
It’s a crucial tool for combatting a virus impervious to borders, seasonality, and many of the lockdown measures employed by anxious nations. So, when US National Institute of Allergy and Infectious Diseases director Anthony Fauci tells Congress, as he did in July, that he’s optimistic a vaccine will be ready in late 2020 or early 2021, it’s tempting to imagine that as the moment when we can once again engage in all the activities that remain laced with fear, like hopping a plane, or seeing a concert, or hugging a grandpa. An effective vaccine represents an enormous, exciting move in that direction. But it’s not the pandemic finish line—it’s more like a pandemic off-ramp. Epidemiological, logistical, and ethical roads still lie ahead: to determine how long and how well that vaccine’s protection can last, to manufacture enough of it to jab into billions of arms, to allocate the first batches of supply between countries and within their populations, and to persuade vaccine skeptics to roll up a sleeve. We’re trying to protect the entire planet, all 7.8 billion of us. “The job isn’t done when you’ve got an effective vaccination,” says Ross Upshur, a professor at the University of Toronto’s Dalla Lana School of Public Health who cochairs the World Health Organization’s COVID-19 ethics working group. “The job is done when you get that vaccine out to everyone who needs it.”
Humans have been trying to outsmart viruses for millennia. By the late 1600s, Chinese doctors had formalized their recipe: grind a smallpox scab into a powder and blow it up a healthy patient’s nose. (Apparently, for boys, this was done in the left nostril, and for girls, the right.) An ambassador to Britain sent reports of seventeenth-century North African surgeons making a small incision between the thumb and forefinger, then squeezing smallpox pus into the wound. At the turn of the nineteenth century, Edward Jenner extracted fluid from a cowpox blister, taken from—who else?—a milkmaid, and scratched it into the arm of an eight-year-old boy. These efforts may seem crude now—we prefer our vaccines packed tidily in glass vials, injected though sterile hypodermic needles—but the idea remains the same: teach the immune system how to ward off a virus so it has a head start should infection occur.
A vaccine is, in essence, a trick—a sleight of hand that convinces your body to mount a counterattack to a given pathogen before that pathogen actually infects you
When a new pathogen invades the human body, our innate immune system recognizes the presence of something noxious and sends up an alarm. The first responders are proteins that meddle with a virus in order to limit its ability to reproduce. “This is what’s called the dumb part of the immune
system, though that’s quite mean because it’s not dumb at all,” says Brian Ward, an infectious-disease professor at McGill University and the medical officer for Medicago. But it’s also not precise: the innate immune system attacks anything that appears foreign and troublesome.
Cue the adaptive immune system. “When cells are infected with a pathogen, they gobble it up, break it into pieces, and then start showing those pieces to the cells, saying, Hey, I found something that doesn’t belong here, can you please get rid of it?” says Marc-André Langlois, a molecular virologist at the University of Ottawa. B cells (a type of white blood cell) begin making antibodies: proteins that can subdue a virus by blocking its ability to get into the body’s cells. T cells (another type of white blood cell) arrive with two purposes: to help B cells make more antibodies and to assassinate cells that have been infected by the virus. It’s a more sophisticated response, but it’s also slower, taking a week, sometimes longer, to mobilize. “So, if you have a rapidly replicating virus, and it doubles, doubles, doubles, waiting seven days for antibodies might be too long and you might not survive,” Langlois says.
If the infection is cleared, many of the body’s B and T cells then die off themselves. Some, though, transform into memory cells, typically bunkered down in your bone marrow, where they wait to spring into action the next time that same pathogen attacks. “All it takes is one B cell to recognize the target and get activated, and it will start proliferating so it can produce the antibodies,” Langlois says. “That’s why vaccines work. They give you this life-saving element of having the antibodies ready to be deployed.” A defence that would otherwise take the body weeks to mount can be summoned in just a few hours.
We’ve come a long way from smallpox pus, but to develop a vaccine, scientists still need to pick their poison. In modern medicine, that decision involves choosing whether to use the entire virus or just a vital part of it. Whole-virus vaccines are the traditional approach. One strategy, dating back to the 1930s, is to take the pathogen—grown in giant batches of chicken eggs or, decades later, in cells—and then kill it, usually with heat, chemicals, or radiation. Because the virus is dead, it doesn’t cause disease once introduced to the body, even in people with weakened immune systems; because the virus is dead, it also doesn’t always cause a strong immune response, often requiring multiple doses. This approach is used in the flu shot and a hepatitis A vaccine, as well as in the one for polio, which a global vaccination effort has essentially wiped out.
In a more recent variation on the whole-virus vaccine, a pathogen is weakened in a lab rather than killed outright. Chances are you’ve been jabbed with a bunch of these vaccines: they’re how we fight measles, chicken pox, yellow fever, and tuberculosis. Here, the cost-benefit analysis is reversed: because the vaccine closely resembles a natural infection, it typically elicits a robust, enduring response; because the vaccine is more potent, though, people with compromised immune systems are often unable to get it at all. But, by using the entire virus, the vaccine builds an immune response to many different parts of the pathogen. “The whole-virus vaccine is like a big shield in front of you,” Ward says. “If you’re in a Star Wars movie and someone is shooting lasers at you, you’re much safer behind that shield.”
Yet a smaller shield, precisely positioned, can still protect you by blocking an important part of the virus rather than the whole thing. There are several ways of introducing this target protein—which is called the antigen—to the body. Most of them require another ingredient to fortify the shield: an adjuvant, usually aluminum, which for the past ninety years has been added to vaccines to boost the immune response. “An adjuvant is a little like hot sauce,” says Robert Kozak, a microbiologist at Toronto’s Sunnybrook Health Sciences Centre. It livens up what’s already on your plate.
One method of delivering the target protein to your body is to deploy a weakened common-cold virus, called an adenovirus, as a microscopic Trojan horse. That cold virus is unlikely to cause much damage, but it’s hugely efficient at slipping inside cells and releasing the antigen. Though scientists see promise in this approach, only one adenovirus vaccine has ever been approved, anywhere. In part, that’s because vaccines tend not to make a ton of money, and it’s wildly expensive to develop a new platform, so funding can be hard to come by. It’s also because adenovirus-vaccine candidates are in human trials for complicated diseases, like HIV and malaria, which are challenging targets.
Another method skips the Trojan horse altogether and injects you directly with the pathogen’s critical protein. Virus-like-particle vaccines, such as Medicago’s plant-grown candidate, are a type of these protein-based vaccines. It’s a proven method—HPV and hepatitis B are just two examples—and there are usually few side effects once you’re given the shot.
Then there are genetic vaccines, which don’t deliver the antigen itself but instead issue a blueprint of that target protein to our bodies, hijacking our own cells to produce it. In a DNA vaccine, DNA containing the gene for the antigen is delivered to the cells. The cells copy those genetic instructions into molecules called messenger RNA (mRNA), which issue marching orders to the body to assemble the antigen.
“The antigen is then presented to the immune system, [which] mounts a defence,” says Gary Kobinger, one of the scientists behind the Ebola vaccine, who is now working on a DNA candidate for a COVID-19 vaccine for Laval University. It’s a relatively new method of vaccination, though Kobinger points out that, “in the field of experimental vaccines, it’s quite old,” a technology discovered back in the early ’90s.
Messenger RNA vaccines bypass the DNA and go straight to the marching orders. The genetic material for the antigen is produced synthetically, then packed inside a pod made of lipid molecules, which slide easily into the cells. The benefits are that there’s no messing around with infectious material and the vaccine’s production time can be cut down dramatically, which is why some researchers believe a genetic vaccine for COVID-19 will be ready first. The disadvantage is that this is uncharted territory: no DNA or mRNA vaccines are currently approved for human use.
SARS-CoV-2 is a stealthy operator. It has a gift for binding its spike proteins—those knobby mushrooms that every coronavirus illustration has burned into our brain —to receptors on particular cells scattered in high numbers along the lining of our respiratory tract. When contact is made, it creates an opening through which the virus can pour its genetic code, the RNA, inside our bodies. “The moment the RNA enters the body, it takes [over] the cell—there’s no wasting time,” says Natalia Martin Orozco, vice-president of drug development at Toronto-based Providence Therapeutics, which pivoted from developing an mRNA vaccine for cancer to one for COVID-19. The first proteins that SARS-CoV-2 produces are not to make more copies of itself but instead to suppress an immune response. “It says, Okay, let’s block everything that is going to stop me from multiplying,” Martin Orozco says. “After that, it starts producing what it needs to build the virus and grow.”
There are now more than 200 vaccine candidates for COVID-19 in development around the world, using every conceivable approach. The vast majority of them, however, zero in on the spike as the vaccine’s target protein: the University of Oxford, Johnson & Johnson, and CanSino Biologics all insert the spike into weakened common-cold viruses; Novavax’s vaccine attaches the proteins to microscopic particles that are used as carriers; Moderna and Pfizer’s candidates encode the spike into their mRNA. It’s a good bet. The spikes are found in abundance on the surface of the virus, so they’re what our immune system sees first. “With the first SARS, we saw that the virus used the spike protein to enter cells,” says Kozak. “Viruses can be shockingly unoriginal sometimes, so if blocking that protein protected you against SARS One, it will probably work against SARS Two.”
Not all of these candidates, in the end, will work—many of them won’t. (A sobering statistic: one 2016 study found that nearly nine out of every ten new drugs fail in the human-testing phase.) And it’s not yet clear what exactly will ward this virus off. “We don’t know the relative importance and contribution of antibodies and T cells in terms of protection against COVID,” says Manish Sadarangani, director of the Vaccine Evaluation Center, in Vancouver. Immunity isn’t an on/off switch: there are multiple levels of protection conferred by either shaking off a disease or receiving its vaccine. Some vaccines, like the one for hepatitis A, provide sterilizing immunity, which prevents the infection and its transmission almost entirely. Others, like those for diphtheria and tetanus, generate neutralizing immunity, where an infection can occur but won’t get very far and can’t make someone sick. Sometimes, as with the shingles vaccine, recipients aren’t fully covered but experience a milder version of the disease. Often, protection isn’t life-long, so we need booster shots to shore up our immunity.
When it comes to coronaviruses, immune responses tend to be short-lived: two to three years for the first SARS virus, for example, after which people exposed to that same pathogen would likely fall sick once again. Still, three years of protection sounds pretty good right now. As Martin Orozco says, “Even if the vaccine lasted just one season, that, to me, would be a really great accomplishment.” In the midst of a pandemic, a SARS-CoV-2 vaccine that performs as well as a flu shot is nothing to sneeze at.
Twice a year a consortium of scientists representing more than 100 influenza centres in more than 100 countries descends on the World Health Organization (WHO) to pick the flu strains that should be combatted by seasonal vaccines. For the northern hemisphere, these selections are made in February; for the southern hemisphere, September. Once the recommendations are made, the viruses are produced in WHO laboratories, then shipped to the companies around the world that manufacture the corresponding vaccines. There is no centralized body whipping up batches of SARS-CoV-2 for developers looking to try their hand at a COVID-19 vaccine. Instead, they need the genetic code for the virus, which Chinese researchers sequenced in the second week of January and shared in a public database. Once scientists determined what was inside the 30,000 “letters” of this coronavirus’s RNA, they could decide which proteins to target in their vaccines.
After developers pick their antigen and their delivery system, they test it, starting with animals. Because ferrets and hamsters are, like us, naturally susceptible to SARS-CoV-2, they were a popular choice for early vaccine trials at the University of Saskatchewan’s Vaccine and Infectious Disease Organization-International Vaccine Centre (vido-InterVac). If the vaccine protects those animals from infection, the next step is a safety trial with dozens of people, to see if fevers spike or injected arms swell, followed by another trial, which measures how well an immune response to the virus has been produced. Then it’s on to the third trial, where thousands of volunteers are monitored for a statistically significant difference between rates of infection in an unvaccinated control group and in people who actually got the jab. At least half a dozen leading candidates have entered phase-three trials, including ones from the University of Oxford, Moderna, and Pfizer. Currently, the WHO has set the minimum bar for an effective vaccine at an infection-reduction rate of 50 percent, though 70 percent is preferred.
What’s needed to make enough doses for these trials depends on the type of vaccine. For Medicago’s plantbased candidate, there must be wellstocked greenhouses and a dunking tank. To take another example: at vido-InterVac, where researchers are working on a protein-based vaccine, they begin with a single cell. “We take the gene from the virus that encodes for the spike protein, and we put that gene into the single cell, which now thinks it is its own protein,” says vido-InterVac director and ceo Volker Gerdts. At first, scientists use a three-litre beaker that contains everything necessary to make a cell happy: some sugars, a couple of amino acids, a nice warm environment, and a little CO2, so the cell is fooled into believing it’s still in a body. One cell divides into two, then four, then eight, then sixteen; the three-litre beaker becomes twenty litres, then 250, all the way up to a 1,000- or 2,000-litre bioreactor. From one individual cell, you can make enough of the protein for thousands, even millions of doses.
Gerdts’s team wants just that protein in its vaccine, without sugar or waste or any of those extra bits. To isolate the spike, the liquid will get separated in a centrifuge: spun so the heavier waste and cell walls fall to the bottom, leaving the lighter protein on top. It will then get purified, so anything else that lingers is removed. “It gets really cleaned up to the point where you just have a very concentrated, pure substance,” Gerdts says. “And then you put it in a glass vial.”
Making a successful vaccine is one challenge. Making enough of it to satisfy world demand is another. There are, of course, all sorts of regulations and standards concerning how to go about production: “I can’t head into my basement and start brewing up a vaccine,” says Curtis Cooper, president of the Canadian Foundation for Infectious Diseases. Every facility needs to conform to Good Manufacturing Practices (gmp), which are exceptionally specific rules set out by the WHO that ensure quality control. You want consistency over time so that each successive batch is precisely the same.
Many Canadian labs can produce enough vaccine for their clinical research under these strict gmp conditions. But, when it comes to scaling up production, we’re not in nearly as strong a position. Gerdts says that there are two facilities in Canada with large-scale production capacity: Medicago and the National Research Council, which partnered with CanSino Biologics to produce its vaccine and received a recent $126 million federal boost. At Medicago’s clinical facility in Quebec City, 20 million doses of its plant-based vaccine, if successful, can roll out over a year; there’s a commercial facility in North Carolina that can manufacture another 100 million doses annually for whoever signs a contract. A third facility is slated to be built in Quebec, with greenhouses the size of two football fields, though that won’t be completed until 2023. And, in March, vido-InterVac received $23.3 million from the Canadian government, half of which will be used to complete its own much larger facility, which should be ready by next July. In the meantime, Gerdts is compelled to wait until another manufacturer can begin to produce his candidate. “Canada does not have the manufacturing capacity that is needed for making a vaccine for the world,” he says. “We’re not even close to making enough for Canadians.”
What happened? Marc-André Langlois believes that—at least before this very moment—there wasn’t much of an appetite to equip the country for a hypothetical pandemic. “It’s generally unpopular to invest in preparedness, because you have all the other urgent commitments that start creeping up,” he says. “People might not want $300 million spent on making a vaccine-manufacturing facility for another virus that could potentially burn out.”
It’s also a predictable outcome of operating in a global economy. “We outsource a lot of our vaccine procurement to these big multinationals in Europe, and we have not invested in the production capacity in Canada,” says vido-InterVac’s associate director of business development, Paul Hodgson. Canadian branches of international pharmaceutical companies, like GlaxoSmithKline and Sanofi Pasteur, are capable of producing other vaccines, but “it’s not like they have extra capacity just sitting there to push a new vaccine through,” he says. “It’s a matter of priorities—when there’s an opioid crisis or roads need repairs, where do you put the money? But, if you think research is expensive, you should try disease.”
That has sent Canada looking for supplies elsewhere. The federal government has ordered 75 million syringes and needles from medical-technology company Becton Dickinson, enough to inoculate nearly every Canadian twice, and issued bids to secure a similar quantity of alcohol swabs, gauze strips, and bandages. “Our government is working on all possible fronts to deliver safe and effective treatments and vaccines to Canadians as quickly as possible,” procurement minister Anita Anand says. “What this means is, while we are working with domestic suppliers, we are also pursuing international arrangements.” In early August, she announced the first of these arrangements: a pair of deals with American companies Pfizer and Moderna for tens of millions of doses of their respective mRNA vaccines. By month’s end, Canada had also secured 38 million doses of Johnson & Johnson’s candidate and 76 million doses of Novavax’s vaccine.
Plenty of other countries inked deals of their own this summer: the UK reserved 100 million doses of the University of Oxford’s vaccine while the US secured another 300 million—that’s nearly a quarter of Oxford’s projected annual supply gone. By mid-August, preorders of COVID-19 vaccine candidates were reportedly stretching toward 6 billion doses, almost all of them claimed by wealthy nations. None of these vaccines has yet been proven to work.
There’s another risk in relying on international sources: the goods might never show up. Early in the pandemic, for example, the White House ordered medical manufacturing titan 3M to stop exporting N95 face masks to Canada and elsewhere until the US shored up its own supply. The clinical trial for CanSino’s vaccine candidate was meant to start in Halifax this past May. Chinese customs refused to release the shipment; by late summer, the trial had to be called off.
Global initiatives do exist to try to level the vaccination playing field. The international immunization nonprofit Gavi is pooling money from dozens of highand middle-income countries to invest in a number of vaccine candidates, including Oxford’s, with the aim of manufacturing 2 billion doses by the end of 2021. That’s meant to be enough for each country to vaccinate 20 percent of its population, with an emphasis on front line workers and vulnerable groups and with the cost fully covered for low-income nations. In June, Canada pledged $120 million to the Access to COVID-19 Tools Accelerator, a global project that includes Gavi’s vaccine-distribution initiative. China and the US haven’t contributed.
But every country, company, and initiative will be competing for the same limited supplies; already, there have been murmurings of glass shortages that could curb the availability of vials. Stoppers are made by only a handful of companies. And it doesn’t take much to cause a major bottleneck. “At the beginning of the pandemic, we didn’t have enough nasopharyngeal swabs for COVID-19 tests,” says Allison McGeer, a senior clinical physician at Toronto’s Sinai Health System. More than 100,000 swabs, ordered by the federal government, arrived in Ontario contaminated by mould. “These are tiny, [cheap] things, but if you don’t have any of them, you’re paralyzed,” she says. “There’s a long list of those things that go into vaccine manufacturing that have a potential to pose the same sort of problems. There only has to be one little grommet missing and the whole system doesn’t work.”
Vaccines are designed to prevent infection. You don’t want to cause another infection altogether by putting that vaccine in a grimy vial. Sterilization is extremely important: this is a product moving from the outside world directly into our muscles. “We have to prepare and sterilize the vial, prepare and sterilize the stopper, all the tubing and fill needles, all the parts and pieces that would touch the vaccine,” says Christopher Procyshyn, cofounder of Vancouver-based Vanrx Pharmasystems. “Everything is individually sterilized and then brought together in an aseptic process, which basically means: don’t screw it up.”
However it has been made, the vaccine arrives at a facility like Vanrx’s in a bag or a tank, frozen or in liquid form. It’s most often sterilized through microfiltration, which passes the product through a filter with pores smaller in diameter than any known bacteria. The glass vials also arrive and are sterilized: washed with purified water, then blasted with heat. “Glass is a greasy material, so we have to take it to a high enough temperature that we burn it off, much like a self-cleaning oven,” Procyshyn says. The vials go into a filling machine, where they’re sterilized using high-pressure steam, as are the stoppers and caps.
In conventional technologies, what happens next “looks a lot like Laverne and Shirley—like a food-processing line,” Procyshyn says. “You have conveyor belts coming in,” and a machine positions a whole bunch of tubes, which, he continues, “squeeze in a pulsation manner and fill the vial with the liquid, the stopper, the cap.” Vanrx automates the process inside a large machine, where the filling is done by a robot. Procyshyn suspects that, given the need to conserve supplies, vaccines for COVID-19 will be packaged in multidose vials, enough to vaccinate twenty patients each. The fastest machines in the industry run around 600 units per minute: for one facility, on a full production day, that translates to somewhere between 15 and 20 million doses. “But don’t forget that other drugs are continuing to be made,” Procyshyn says. “Not all facilities are suitable for this, and Canada has fewer . . . than the US and Europe. A large part of what we’re working through right now is which vaccine at which available site and what capacity.”
Now ensconced in its multidose vial, the vaccine is inspected by employees, labelled, and given a lot number, essential for safety tracking. After that, it has to be transported through the cold chain, a standard practice to ensure that, every time the vaccine is handed off, it maintains the appropriate temperature, typically between 2 and 8 degrees for refrigerated vaccines or -15 degrees for frozen ones.
That means the moment it leaves the doorstep of the manufacturer, bundled in boxes wrapped in isothermal packaging, the vaccine is kept in chilly containers. The plane that transports it is refrigerated, as is the truck that picks it up from the airport, as is the wholesaler or warehouse in Canada where it’s kept before being moved to health care facilities across the country. “This is a well-established process,” says Mina Tadrous, an assistant professor at the University of Toronto’s Leslie Dan Faculty of Pharmacy. “We’ve been doing this for decades and we’re really good at it.”
No one needs to rely on the diligence of others: surveillance systems exist to make sure that the cold chain hasn’t been broken. “It used to be that you’d carry in a box of vaccines, and there was a temperature probe inside that provided a continuous recording, so you’d make sure they hadn’t been frozen or gotten too hot,” McGeer says. Then, in 1996, the WHO introduced temperature-sensitive stickers that monitor the heat exposure of individual vaccine vials. “It’s a stellar development: a little colour-coded square that tells you whether it’s been out of temperature,” she says. The square starts lightly tinged; if it gets dark, the vial needs to be discarded. As a result, clinicians can determine whether the whole box has been compromised or just a few vaccine vials fell out of the cold chain. When supply is tight, it helps to have every possible vial on hand.
We might be inventing a vaccine from scratch, but we’re not inventing a whole new system to get it into the arms of Canadians. “The best immunization system is almost invisible,” says Natasha Crowcroft, inaugural director of the University of Toronto’s Centre for Vaccine Preventable Diseases and now a senior technical adviser at the WHO. “People talk about immunization being the victim of its own success: when everything is going smoothly, no one knows how much work goes on behind the scenes.” In Canada, this work involves a terrific amount of coordination between the federal government, responsible for procuring the vaccine; the provinces and territories, which determine how many doses they’ll need and which ones to deliver to which people; and local jurisdictions, which make on-the-ground decisions about administering it.
When it comes to distributing vaccines for COVID-19, Canada will most likely take cues from the influenza-vaccination programs we have in place. For those, Health Canada approves and then bulk orders the vaccines, choosing a couple of different candidates in case there are manufacturing snafus or to target certain segments of the population—seniors tend to get a high-dose flu shot because their immune systems benefit from the added boost. Buying in bulk helps cushion the cost: Moderna, which has said it plans to make a profit from its SARS-CoV-2 vaccine, will lower the price for big orders. The provinces then determine how exactly to get the doses out, allotting a certain share to family doctors, public health clinics, community clinics, and pharmacies. Typically, they’ll also decide whether they will publicly fund vaccination and for whom. Ontario has a universal flu-vaccination program, for example, and BC and Quebec do not, though it’s hard to imagine that anyone will have to shell out for a COVID-19 shot.
While flu shots are ordered and distributed based on how many people got one the previous year, planning for COVID-19 vaccines presents its own challenges: we don’t know what the supply is going to be, how well it will work in different populations, or how many doses the vaccine might require. “If they’re anticipating that we’re going to have tons of doses in a short period of time, then it would make sense to have as many vaccinators as possible,” says Jeff Kwong, epidemiologist and interim director of the Centre for Vaccine Preventable Diseases. You could walk into your family doctor’s office, the local library, the nearest Shoppers Drug Mart or Pharmasave—take your pick. “But, if they’re going to have relatively low numbers of doses available each week, then having a more limited number of vaccinators is more efficient.” You don’t want to run into a situation where one physician has fifty doses sitting idly in a fridge while another scrambles to contend with an out-the-door line.
For that reason, vaccines could be administered just in public health clinics. “After the H1N1 pandemic, we really spent a lot of time developing our mass-immunization clinic plan,” says Toronto’s associate medical officer of health, Vinita Dubey. “That was the time to detail some of the boots-on-the-ground logistics.” The plan includes everything from where to hold large vaccination clinics and how to keep them staffed to strategies for managing lines and signage for orienting people. “It’s not like we don’t have experience doing this,” Kwong says. “It’s about preparing for multiple scenarios and trying to be as responsible as possible.”
In fact, administering the flu shot this influenza season will be a good trial run for getting out a COVID-19 vaccine. Although physical-distancing measures and travel restrictions might mean a milder flu season, health care officials in Canada are expecting higher demand this winter. “We know we will have smaller, more frequent clinics because large clinics become a large gathering,” Dubey says. Expect longer hours, assigned appointments, and perhaps even at-home vaccinations, especially for high-risk or vulnerable people. “We’re also reimagining our school-based clinics because we know that doing vaccines in schools is going to look different this year,” she says. “That’s preparation for COVID-vaccine planning for sure.”
We are, by now, well accustomed to thinking in waves: waves of COVID-19 infections, waves of lockdown measures, waves of fear and fatigue. Almost certainly, we will also have to contend with waves of vaccination as batches roll off manufacturing lines or we wait for new candidates to be approved. Still, someone is going to be first to pull up a sleeve. “We want the vaccine now, and we want enough for everybody,” McGeer says. “But, if we have enough vaccine for 5 percent of the population, then who will be that 5 percent?”
The National Advisory Committee on Immunization (NACI), formed back in 1964 to review administering the polio vaccine, among others, makes recommendations on immunization practices and schedules, including which populations should get the vaccine first. “We look at age-specific risks for disease and complications, the ability of people to respond to the vaccine according to age, and whether there is a risk because of occupation,” says NACI vice-chair Shelley Deeks. “Not only do we want to protect the vulnerable but, because this a pandemic, we want to ensure essential services can continue.”
NACI advises on priorities, but because health care is a provincial responsibility, it’s up to the provinces and territories to actually implement those recommendations. “There are real differences that might result in different strategies based on where you are,” Mc-Geer says. “Who you target in Nunavut is not the same as in downtown Toronto.” The expectation is that provinces have a closer eye on the particular needs of their communities.
And it’s the provinces that actually set most of the disease-control goals. Do you vaccinate to prevent mortality? In that case, for this virus, the elderly need to be prioritized. Do you vaccinate to reduce transmission and spread? There are some house-partying twentysomethings in Kelowna who could get the jab. Or do you vaccinate widely in an attempt to achieve herd immunity? NACI advises that front line workers be prioritized because they’re at a greater risk of infection based on the work they do. But that’s not axiomatic: “There’s no commandment in the bible of pandemic response that health care workers go first,” Upshur says. “You have to make arguments, and those arguments are based partly on data and partly on ethics.” We know that racialized and low-income people are infected at rates wildly disproportionate to their populations, not for any epidemiological reason but because of historical and economic disadvantages. This inequality persists for those working in the health care system itself: The Lancet published a study of almost 100,000 front line health care workers in the UK and US, which found that racialized workers were nearly twice as likely as their white colleagues to come down with COVID-19. Should decision making about vaccine prioritization be based on structural social causes instead?
But history complicates that approach as well: a long tradition of surveillance and systemic discrimination in the health care system gives racialized people a very good reason not to want to go first. “In a public health emergency, where you’re using a vaccine that doesn’t have a lot of safety and effectiveness data, there’s obviously some concern about giving it to the most vulnerable groups, who might feel they’re being used as guinea pigs,” says Alison Thompson, an associate professor at the University of Toronto’s pharmacy school whose research focuses on the ethics of vaccines. “I think it’s really about being as transparent as possible through this entire process of development, manufacturing, and distribution. People need to be able to see what’s in the needle.” That transparency could also help persuade the one in six Canadians who currently say they would not get the vaccine.
Though it can feel like this virus has been with us for roughly eight centuries, it’s not yet been twelve months. In that time, a few hundred vaccine candidates have been created, dozens have entered human trials, and pretty much every promising new technology has been pressed into action. Work that would normally occur in sequence and stall on some bureaucrat’s desk is now, thanks to huge financial investments by governments around the world, happening swiftly and in tandem. “The speed is not from sacrificing safety,” the WHO’s Crowcroft says. “It’s sacrificing money.” That still won’t buy an end to this pandemic as quickly as we’d like: there’s much mask-wearing and social distancing and staying home ahead. But the average new vaccine takes about a decade to make it to market. The fastest ever to make it to market, for mumps, arrived in four years. We’re virtually guaranteed to shatter that record for COVID-19—one more unprecedented event in an age already full of them.





